 NETs:
NETs:
Up to 60% of pancreatic neuroendocrine tumors are nonsecretory or nonfunctional, which either do not secrete, or the quantity or type of products such as pancreatic polypeptide, chromogranin A, and neurotensin do not cause a clinical syndrome, although blood levels may be elevated.
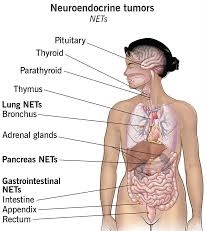
Rarer forms of neuroendocrine tumors that arise anywhere in the body, including within the lung, thymus and parathyroid.
Bronchial carcinoid can cause airway obstruction, pneumonia, pleurisy, difficulty with breathing, cough, and hemoptysis. ,
Most pancreatic NETs are sporadic.
However, neuroendocrine tumors can be seen in several inherited familial syndromes:i
multiple endocrine neoplasia type 1 (MEN1)
multiple endocrine neoplasia type 2 (MEN2)
von Hippel-Lindau (VHL) disease
neurofibromatosis type 1
tuberous sclerosis
Carney complex
NETs are believed to arise from various neuroendocrine cells.
Neuroendocrine cells function is to serve at the neuroendocrine interface.
Neuroendocrine cells are present not only in endocrine glands throughout the body that produce hormones, and in all body tissues.
Symptoms from secreted hormones advanced
Aside from the hormones of secretory tumors, the most important markers are:
chromogranin A (CgA), present in 99% of metastatic carcinoid tumors.
urine 5-hydroxyindoleacetic acid (5-HIAA)
neuron-specific enolase (NSE, gamma-gamma dimer)
synaptophysin (P38)
N-terminally truncated variant of Hsp70 present in NETs
High levels of CDX2, a homeobox gene product essential for intestinal development and differentiation, are seen in intestinal NETs.
Neuroendocrine secretory protein-55, a member of the chromogranin family, is seen in pancreatic endocrine tumors but not intestinal NETs.
CT-scans, MRIs, sonography and endoscopy, including endoscopic ultrasound are commonly used imaging techniques for diagnostics and for evaluation of therapy.
Neuronedocrine tumors express somatostatin receptors providing a target for imaging.
OctreoScan, also called somatostatin receptor scintigraphy utilizes intravenously administered octreotide that is chemically bound to a radioactive substance, often indium-111, to detect larger lesions with tumor cells that are avid for octreotide.
Somatostatin receptor imaging can now be performed with positron emission tomography (PET).
Gallium-68 receptor PET-CT is much more accurate than an OctreoScan.
Imaging with fluorine-18 fluorodeoxyglucose (FDG) PET may be valuable to image some neuroendocrine tumors.
Imaging with fluorine-18 fluorodeoxyglucose (FDG) PET help assess the aggressiveness of the tumor.
Gallium-labelled somatostatin analog and 18F-FDG PET tracers ensures better staging and prognostication of neuroendocrine tumors.
NETs show tissue immunoreactivity for markers of neuroendocrine differentiation and may secrete various peptides and hormones.
Neuroendocrine tissue markers are various chromogranins, synaptophysin and PGP9,
Neuron-specific enolase (NSE) is less specific.
The nuclear neuroendocrine marker insulinoma-associated protein-1 (INSM1) has proven to be sensitive as well as highly specific for neuroendocrine differentiation.
NETs are often small, yellow or tan masses.
NETs are often located in the submucosa or more deeply intramurally.
NETs can be very firm due to an accompanying intense desmoplastic reaction.
NETs overlying mucosa may be either intact or ulcerated.
Histologically, NETs show uniform cells which have a round to oval stippled nucleus and scant, pink granular cytoplasm.
NET cells may align variously in islands, glands or sheets.
Electron microscopy can identify secretory granules.
MInimal pleomorphism is present, but less commonly there can be anaplasia, mitotic activity, and necrosis.
Some neuroendocrine tumor cells possess especially strong hormone receptors, such as somatostatin receptors and uptake hormones vividly.
NETs from a particular anatomical origin often show similar behavior as a group, such as foregut, midgut and hindgut.
Foregut NETs are argentaffin negative, and often secrete 5-hydroxytryptophan (5-HTP), histamine, and several polypeptide hormones.
Foregut NETs may be associated atypical carcinoid syndrome, acromegaly, Cushing disease, other endocrine disorders, telangiectasia, or hypertrophy of the skin in the face and upper neck.
Foregut NETs can metastasize to bone.
Midgut NETs are argentaffin positive, can produce high levels of serotonin 5-hydroxytryptamine (5-HT), kinins, prostaglandins, substance P (SP), and other vasoactive peptides, and sometimes produce corticotropic hormone.
Bone metastasis is uncommon with midgut NETs.
Hindgut NETs are argentaffin negative and rarely secrete 5-HT, 5-HTP, or any other vasoactive peptides.
Bone metastases are not uncommon in Hindgut NETs.
Treatment of a neuroendocrine tumor considers: its location, invasiveness, hormone secretion, and metastasis.
Treatments may be aimed at cure or at palliation.
If the tumor is locally advanced or has metastasized, but is slowly growing, treatment that relieves symptoms may often be preferred over immediate challenging surgeries.
Intermediate and high grade tumors are usually best treated by various early interventions rather than observation.
In malignant carcinoid tumors with carcinoid syndrome, median survival is more than eight years.
Surgery often has a role in neuroendocrine cancers for palliation of symptoms and possibly increased lifespan.
Cholecystectomy is recommended if there is a consideration of long-term treatment with somatostatin analogs.
In secretory neuroendocrine tumors, somatostatin analogs given subcutaneously or intramuscularly alleviate symptoms by blocking hormone release.
Somatostatin analogs may also stabilize or shrink tumors: study on the antiproliferative efficacy of Octreotide LAR in patients with metastatic neuroendocrine MID gut tumors has an average tumor stabilization was 14.3 months compared to 6 months for placebo.
The CLARINET study (a randomized, double-blind, placebo-controlled study on the antiproliferative effects of lanreotide in patients with enteropancreatic neuroendocrine tumors has demonstrated the antiproliferative potential of lanreotide, a somatostatin analog.
Interferon’s effectiveness is somewhat uncertain, and is often used in combination with other agents.
Most gastrointestinal carcinoid tumors tend not to respond to chemotherapy agents, with 10 to 20% response rates that are typically less than 6 months.
Combining chemotherapy medications has not usually been of significant improvement: 25 to 35% response rates that are typically less than 9 months.
With poorly differentiated, high-grade or anaplastic, metastatic disease, and Somatostatin Receptor Scintigraphy (SSRS) negative tumors cisplatin with etoposide have a response rate in excess of 70% compared to 10% in strongly positive SRSS carcinoid tumors.
Targeted therapy with everolimus (Afinitor) and sunitinib (Sutent) is approved by the FDA in unresectable, locally advanced or metastatic PanNETs.
Combining several medicines, particularly doxorubicin with streptozocin and fluorouracil is often effective.
Although marginally effective in well-differentiated PETs, cisplatin with etoposide is active in poorly differentiated neuroendocrine cancers.
Radionuclide therapy is a type of radioisotope therapy in which a peptide or hormone conjugated to a radionuclide or radioligand is given intravenously, the peptide or neuroamine hormone previously having shown good uptake of a tracer dose.
The peptide receptor may be bound to radioisotopes lutetium-177, yttrium-90, indium-111 and other including alpha emitters.
Radionuclide therapy is a highly targeted and effective therapy with minimal side effects in tumors with high levels of somatostatin cell surface expression.
The radiation is absorbed at the sites of the tumor, or excreted in the urine.
The radioactively labelled hormones enter the tumor cells which together with nearby cells are damaged by the attached radiation.
Not all cells are immediately killed, as cell death can go on for up to two years.
Hepatic artery embolization (HAE) occludes the blood flow to the tumors, achieving significant tumor shrinkage in over 80%.
In hepatic artery chemotherapy, the chemotherapy agents are given into the hepatic artery, often by steady infusion over hours or even days.
Compared with systemic chemotherapy, a higher proportion of the chemotherapy agents are (in theory) delivered to the lesions in the liver.
Hepatic artery chemoembolization (HACE), sometimes called transarterial chemoembolization (TACE), combines hepatic artery embolization with hepatic artery chemoinfusion.
Microspheres bound with chemotherapy agents are injected into the hepatic artery, lodge in downstream capillaries.
The spheres block blood flow to the lesions,and halt the chemotherapy agents in the neighborhood of the lesions, providing a much better targeting leverage than chemoinfusion provides.
Selective internal radiation therapy (SIRT)[for neuroendocrine metastases to the liver delivers radioactive microsphere therapy (RMT) by injection into the hepatic artery, lodging in downstream capillaries.
The nnual incidence of clinically significant neuroendocrine tumors is approximately 2.5–5 per 100,000: two thirds are carcinoid tumors and one third are other NETs.
The prevalence has been estimated as 35 per 100,000.
An autopsy study of the pancreas in people who died from unrelated causes discovered a high incidence of tiny asymptomatic NETs: Routine microscopic findings NETs in 1.6%, and multiple sections identified NETs in 10%.
Enterochromaffin cells, give rise to carcinoid tumors.
Neuroendocrine cells sometimes produce various types of hormones and amines, and they can also have strong receptors for other hormones to which they respond.
Distinguishing between well-differentiated (low and intermediate-grade) and poorly differentiated (high-grade) NETs.
Cellular proliferative rate is of considerable significance in this prognostic assessment.
