 Embryonic malignancy of the sympathetic nervous system.
Embryonic malignancy of the sympathetic nervous system.
A primitive neoplasm of neuroectodermal origin, composed of neuroblast, or immature nerve cells.
These lesions may occur anywhere in the sympathoadrenal neuroendocrine system, including the adrenal gland, connective/soft tissue, retroperitoneum, and mediastinum.
some patients have spontaneous regression of disease without treatment, and other patients have aggressive, metastatic disease requiring multimodal intervention.
The most common extracranial solid tumor in children.
It is responsible for 11% of all deaths from cancer in the pediatric population.
It estimated that more than 700 patients are diagnosed with neuroblastoma annually in the US.
The prevalence is approximately one for 7000 live births
The average age of a patient at the time of diagnosis is between one and two years.
The vast majority of individuals or less than four years of age at diagnosis.
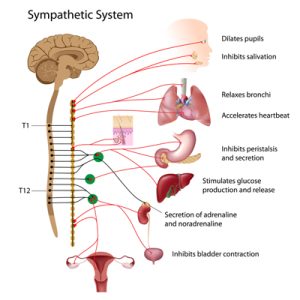
A manifestation of aberrant sympathetic nervous system development.
Arises in cells derived from the neural crest, and it predominantly affects young children.
Its prognosis is poor and treatment is burdensome.
Black patients have a decreased five-year survival rate.
A neuroblastoma, is a neuroendocrine tumor of any neural crest tissue of the sympathetic nervous system.
Arises in sympathetic ganglia or the adrenal glands with propensity to metastasize to lymph nodes, bone, bone marrow, liver and rarely, to lungs and CNS.
Cancer of early childhood.
Accounts for 8-10% of childhood cancers.
Accounts for 10-12% of deaths from malignancy in childhood.
Familial neuroblastoma is rare estimated to be about 1 to 2% of cases.
Histologically demonstrates variation with primitive cells without neuronal features to neurons or ganglion cells.
Behavior and outcome of tumor related to genomic changes.
Symptoms vary depending on the location of the tumor.
Patients with neuroblastoma, most commonly present with abdominal mass or abdominal distension.
Patient may present with appetite loss, weight, loss, irritability, constipation, fever, hypertension, anemia, paralysis, bruising around the eyes, bone pain, and pancytopenia.
Opsoclonus-myoclonus-ataxia syndrome, a paraneoplastic syndrome can be associated with neuroblastoma.
Almost half patients have high risk disease at diagnosis, and the five-year event free survival among these patients is 40 to 50%.
Subsets of children with minimal treatment, have cure rates opposed to 100%.
For patients with high risk disease, the cure rate is approximately 50%.
In children in whom the first line therapy fails, there is a low probability of recovery with subsequent management.
Patients who fail first line therapy, have a long-term survival of approximately 5 to 10%.
11q deleted neuroblastomas grow slowly and respond slowly if at all.
Neuroblastoma cells, express high levels of the disialogangloside GD2, and the targeting of disialogangloside GD2 with monoclonal antibodies is associated with a significant increase in survival among high risk patients.
This indicates the sensitivity of neuroblastoma to immunotherapy and the relevance of the target antigen.
A subgroup cases have autosomal dominant inheritance.
Approximately 800 cases are diagnosed in the US each year, and about half are determined to have high-risk disease.
Long-term survival of children with high risk neuroblastoma is in the 50 percentile.
Risk stratification considers patient’s age, stage, histology, and genomic features which allows the delivery of therapy based on the likelihood of disease recurrence.
Most cases hereditary disease have activated mutations in the tyrosine kinase domain of the anaplastic lymphoma kinase (ALK) oncogene (Mosse YP et al).
Germ line mutations in code for single base substitutions in the kinase domain activating the kinase and a premalignant state.
Oncogene activation mutations can be somatically acquired in 5-15% of cases.
Sporadic or familial cases in conjunction with congenital central hypoventilation syndrome, Hirschsprung’s disease, or both usually have loss of function mutations in the homeobox gene PHOX2B (Mosse YP et al, Trochet D et al).
Genetic testing for ALK mutations and PHOX2B should be considered for patients with a family history of neuroblastoma or lesions suggestive of transmissible mutations such as patients with bilateral primary tumors of the adrenal gland.
Amplification of MYC-N oncogene occurs in about 20% of patients.
The most common presentation for stage for disease is nonspecific symptoms including irritability, fevers, bone pain and limpness.
Local regional disease is often diagnosed accidentally when an abdominal masses palpated, or chest x-ray shows a thoracic mass.
Rarely patients present with paraplegia secondary to paraspinal involvement.
A rare presentation includes the opsoclonus myoclonus syndrome, where patients present with ataxia, myoclonic jerks and nystagmus.
Patients with vasoactive intestinal peptide secretions may present with severe diarrhea.
Patients may present with hypertension related to elevated urinary catecholamines.
The 4-S neuroblastoma is a rare entity with spontaneous resolution, a stage 4 disease in newborns or early infancy, with hepatomegaly and possibly respiratory distress as a result, occasionally noted are skin nodules called the blue berry muffin rash.
Diagnosis confirmed by biopsy and also demonstration of an elevated urinary catecholamines in the presence of bone metastases.
Diagnosis requires tissue acquisition, bone marrow aspiration may demonstrate tumor cells and findings have increased levels of urinary catecholamine metabolites.
Urine catecholamine levels are elevated in the majority of patients with neuroblastoma.
High levels of ferritin and LDH are associated with worse prognosis.
Along with typical imaging techniques of CT scans or MRIs the metaiodobenzylguanidine scan (MIBG) is performed, as the latter is the gold standard diagnostic imaging test.
The MIBG scan can detect primary and metastatic lesions in more than 90% of patients.
Bone marrow examination at multiple sites is required to diagnose and stage patients adequately.
MYCN gene amplification was a independent prognostic marker prior to high dose induction chemotherapy.
MYCN amplification and widespread metastases in patients older than 18 months are characterized as high-risk disease.
For local regional disease diploid tumors have the worst prognosis.
Prognostic markers include 11q deletions and 17q gain in local regional disease, along with LDH and serum ferritin levels, and ratio of urine vanillyl mandelic to homovanillic acid levels.
Mutations in the anaplastic lymphoma kinas (ALK) gene appear to be responsible for the majority of cases of the inherited version of childhood disease, and also plays a role in high risk forms of noninherited neuroblastoma.
Cell of origin is an incompletely committed precursor cell from the neural-crest tissues (Hoehner JC).
In sporadic cases malignant transformation is a result of interaction DNA variants with relatively modest effect on susceptibility.
Median age at diagnosis is 17 months.
Lesions arise in the sympathetic nervous system tissues usually the adrenal medulla and paraspinal ganglia.
Can present as a mass in the neck, chest, abdomen or pelvis.
Presentation is variable from an asymptomatic mass to locally advanced invasive disease, and to widely disseminated tumor.
The most common malignancy diagnosed during the first year of life.
Incidence 10.2 cases per million children under the age of 15 years (Ries LAG).
Associated with one of the highest rates of spontaneous or complete regression of disease (Carlsen NL, Cole WH, Yamamoto K)
Most common extracranial solid tumor in children.
About 800 new cases of all forms of disease occurs annually.
Accounts for 15% of childhood cancer deaths
Localized disease in infants have a 90% survival rate except in cases of Myc-N amplification, where survival is less than 30%.
Metastases found in >50% of children at the time of diagnosis and confers a poor prognosis.
Frequently metastatic to bone, bone marrow and liver at the time of diagnosis.
Approximately 50% of cases that occur in children older than 1 year are associated with metastases at diagnosis.
Age is a continuous variable in terms of prognosis, and 12 or 18 months of age is cut off, as younger patients are more likely to have a benign biological clinical course.
Older children with stage IV metastatic disease her at high risk for death from refractory disease.
Cure rate for children over 18 months with stage 4 disease is approximately 35-40%, and a five year survival rate of approximately 50%.
In patients with localized tumors are almost always cured, even without cytotoxic therapy.
Treatment strategy for high risk neuroblastoma includes induction chemotherapy with well-known toxicitirs and efficacy administered to control metastases and render the primary tumor resectable, followed by surgery for complete resection and consolidation with myeloablative therapy to eradicate resistant clones and maintenance treatment to control minimal residual disease with different agents.
Patients with high risk disease, often undergo induction therapy with multiagent chemotherapy, and surgical resection, followed by consolidative therapy involving high-dose chemotherapy with hematopoietic stem cell rescue and radiation therapy.
Maintenance therapy with an anti-didialoganglioside (GD2) antibody and isotretinoin is also administered.
Approximately half of newly diagnosed patients with neuroblastoma have none high risk disease. Patients with low and intermediate risk neuroblastoma have excellent survival rates,90-95%.
In patients with large primary lesions with localized disease chemotherapy is indicated to attempt surgical excision.
In patients with low risk disease treatment involves surgical resection.
Intermediate risk treatment involves a combination of moderate intensity multiagent chemotherapy and surgical resection.
Approximately half of newly diagnosed patients with neuroblastoma have high risk disease with an estimated five year event free survival rate of 51%.
In patients with high risk disease current therapy includes: induction therapy consisting of multiagency chemotherapy and surgery, consolidation therapy composed of high-dose chemo therapy with autologous stem cell rescue and external beam radiotherapy, and post consolidation immunotherapy directed at minimal residual disease.
Treatment duration is greater than one year.
Patients who present with metastatic disease have a 5-year survival of 30%, despite intensive chemotherapy or stem cell transplantation.
Standard treatment for high risk disease includes dose-dense or dose intensive induction, as well as myeloablative treatments with alkylating agents, platinum agents, topoisomerase II inhibitors , surgery and radiation.
Use of high dose chemotherapy followed by hematopoietic stem cell transplantation and maintenance treatment with retinoic acid improves survival by 35% in metastatic disease, but 5 year event free survival remains less than 50%.
Incidence of leptomeningeal or CNS parenchymal disease in patients who recurrence ranges form 1-16%.
Survival for patients with high risk disease is up to 38%.
Survival for low risk subgroup is more than 95%.
5 year survival rates have increased from 52% during the period 1975-1977 to 74% from 1999-2005, but this improvement is due mainly to increased cure rates among patients with the more benign form of the disease, and the rates among children with high risk disease there has been only moderate improvement in survival (Maris JM et al).
Patients who do not have a partial response to chemotherapy or who have residual bone marrow disease after induction therapy have a survival rate of below 10%.
Treatment for local regional disease is resection of the tumor alone.
For patients with local regional disease and MYCN amplification and for stage 4 disease at greater than 18 months regardless of MYCN amplification, the treatment is very high doses of chemotherapy for induction, followed by surgical resection and then radiation to prevent local recurrence.
To prevent systemic recurrence autologous transplant either preceded by myeloablative chemotherapy ot follow by antibody therapy targeted to GD2 antigen is administered.
If patients receive a complete remission following induction chemotherapy and surgery, patients may be given immunotherapy without myeloablative chemotherapy.
Immunotherapy with 2 anti-GD2 antibodies can prevent recurrence, and chimeric anti-body 14.18 improves progression free survival at two years and is presently the standard of care at transplant (YU AL et al).
3F8 is another anti-GD2 anti-body that is shown long-term event free survival of 50-55% in patients who received first remission.
Alkylating agents are the mainstay of treatment.
Agents utilize including the chemotherapy drugs cyclophosphamide, doxorubicin, vinristine, cisplatin, and etoposide.
Tandem autologous transplant after induction chemotherapy results and better event free survival than single transplant resulting in three-year event free survival 61.6% versus 48.4% (Park JR).
A phase III trial in the children with high-risk metastatic given intense dosing of busulfan-melphalan showed a 49% event free survival compared to 33% for combination carboplatin, melphalan and etoposide, establishing a new standard of care for high-risk neuroblastoma.
2100 Gy is that those of local radiation required for prevention of local recurrence.
Patients with isolated CNS recurrence may be treated with radio immunotherapy, and now patients can be cured or at least receive long-term remissions in an entity that was previously fatal.
Naxitamab-gqgk is approved in combination with granulocyte-macrophage colony-stimulating factor as a treatment for pediatric patients 1 year of age and older and adult patients with relapsed/refractory high-risk neuroblastoma in the bone or bone marrow who have demonstrated a partial response, minor response, or stable disease to prior treatment.
CAR-T therapy with GD2 cells appears effective in early trials.
