 A heterogeneous process characterized by extensive variability in clinical presentation and subsequent evolution.
A heterogeneous process characterized by extensive variability in clinical presentation and subsequent evolution.
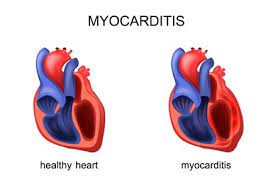
Refers to an inflammatory injury of the myocardium that can involve the cardiac conduction system and pericardial layers.
It affects approximately 4 to 14 people per hundred thousand people per year globally.
Factors associated with acute myocarditis include: family history of myocarditis or cardiomyopathy, recent exposure to drugs, such as clozapine or immune checkpoint inhibitors, vaccines, toxic substances, and certain infections.
Myocarditis may occur in patients infected by parasites after ingesting, raw meat, in patients who have traveled to areas with dengue is endemic, and in patients with Lyme disease.
Acute myocarditis is characterized by acute onset of chest pain, dyspnea, palpitations, occasional syncope, and presence of myocardial infiltrates in the setting of nonischemic cardiomyocyte necrosis on an endomyocardial biopsy or autopsy.
Most patient presents with a prodrome, such as flu like symptoms, respiratory tract symptoms, cough, fever, fatigue, and gastrointestinal symptoms of nausea, vomiting, and abdominal pain.
Acute myocarditis may cause chest pain, shortness of breath, palpitations, and rarely fainting.
Approximately 7% of cases of myocarditis are related to autoimmune disorders.
Myocarditis begins with an immune mediated injury to the myocardium.
Immune cell activation leads to progression of inflammation, contributing to pathological remodeling of the myocardium and dysfunction.
Genetic variants associated with dilated or a rhythmic cardiomyopathies occur in 8-16% of patients with myocarditis..
Approximately 1% of patients with cancer, treated with immune checkpoint inhibitors experience acute myocarditis.
An inflammatory disease of the myocardium diagnosed on the basis of established histologic, immunologic and immunohistchemical criteria.
Mortality from acute myocarditis is approximately one to 7%.
Uncomplicated, acute myocarditis associated with in hospital mortality rates of approximately zero, while patients with complicated acute myocarditis experience mortality or need transplant during hospitalization of approximately 12 and 15% at five years follow up.
Myocarditis recurrence or ventricular arrhythmia occur in approximately 3 to 9% over a period of follow of 19 to 90 months.
Patients hospitalized with COVID-19 and definite or probable acute myocarditis had a 120 day mortality of 6.6%.
Mortality in patients with acute myocarditis and COVID-19 vaccine is approximately one percent.
Previously endomyocardial biopsy was the standard method of diagnosis, which has now been replaced by highly sensitive troponins and cardiac magnetic resonance imaging.
The combination of symptoms, signs, laboratory testing and imaging is now sufficient to establish the diagnosis.
Patients with acute myocarditis myocarditis typically have elevated troponins levels, and inflammatory markers, such as C reactive, protein, and they have ECG changes of ST-T segments, and echocardiographic wall motion, abnormalities particularly in the inferior and lateral walls: cardiac MRI, with or, without endomyocardial biopsy, is necessary to confirm the diagnosis.
Non-invasive cardiac MRI is typically preferred over endo myocardial biopsy.
Fludeoglucose positron emission tomography can also diagnose sarcoidosis and systemic autoimmune disease myocarditis.
Prior to the Covid-19 pandemic the incidence of myocarditis was 1 to 10 cases per hundred thousand persons per year.
Causes of myocardial myocarditis include viruses, such as coronavirus, influenza, parvovirus B19, autoimmune disorder, such as SLE, drugs such as checkpoints immune inhibitors, and vaccines, such as mRNA Covid vaccine or smallpox vaccine.
Myocarditis is uncommon in Covid-19 but almost 39% of patients with myocarditis had a fulminant presentation.
COVID-19 vaccines are rarely associated with myocarditis and occurs mostly in young men, usually self limited: usually after the second dose.
Previously the highest risk was among people between 20 and 40 years of age and among men.
Men make up 60 to 80% of patients with myocarditis.
Women with myocarditis present at older ages.
In the age group 35 to 39 years, the myocarditis rate was 6.1 cases per hundred thousand men and 4.4 cases per 100,000 women, with similar rates in the 20 to 44 year old age group.
The use of cardiac MRI has increased the incidence of myocarditis in the United States from 9.5 to 14.4 per hundred thousand persons.
Cardiac MRI is a noninvasive alternative to identify myocardial edema.
The incidence of myocarditis among patients with heart failure varies from 0.5 to 4.0% according to age and region.
Approximately 25% of patients with myocarditis have left ventricular systolic dysfunction, ventricular, arrhythmias, or heart failure.
Among patients presenting to the emergency room with chest pain 3% have acute myocarditis and pericarditis.
It may resolve spontaneously, cause sudden cardiac death, or evolve into a dilated cardiomyopathy.
Diagnostic criteria include: new onset heart failure, diagnostic changes on a stress test, Holter monitoring, elevated biomarkers and MRI criteria in the presence of normal coronary arteries.
Likely to be present in the presence of life threatening ventricular arrhythmias in the absence of structural heart disease.
Can be triggered by multiple causes: viruses, bacteria, parasites among infectious diseases, autoimmune diseases, hypersensitivity, high catecholamine states, drugs, toxic substances, or physical agents.
May be the result of a hypersensitivity reaction, or reaction to the inhibition of immune checkpoints.
May be seen in the use of checkpoints inhibitors.
Most cases are due to common viruses such as coxsackievirus.
Multiple pharmacological agents are associated with myocarditis: antipsychotic agents, cytotoxic drugs, immuno therapy, vaccines, and salicylates.
Vaccine induced myocarditis has been related to smallpox, anthrax, influenza and Covid-19 MRA vaccines.
Vaccine associated myocarditis is often an eosinophilic one.
Myocarditis with the use of combination immune checkpoint inhibitor therapy has been increasing.
Autopsy examinations in young adults having demonstrated that acute myocarditis was responsible for 3-12% of cases of sudden cardiac death.
Most cases in clinical practice or attributable to viral infections and/or immune reactions.
A viral infection remains the most probable cause of idiopathic myocarditis even when no viruses are detected by serologic or polymerase chain reaction analyses.
In the past 30 years there has been an epidemiologic shift from traditional cardiotropic viruses to parvovirus B19 and HHV-6.
Viral entry into cardiac myocytes occurs through a transmembrane receptor, with necrosis, apoptosis, and activation of innate immunity at 1 to 7 days.
A viral DNA copy number that exceeds a threshold of 500 copies per microgram has been proposed for establishing a virus as the cause of myocarditis.
Viral replication and activation of acquired immune responses with T cell infiltration and autoantibodies occurs at 1 to 4 weeks, and results in either viral clearance or evolution toward dilated cardiomyopathy at months to years.
In such cases when viruses cannot be detected it is presumably due to the fact that the immune system is already achieved complete clearance of the virus.
Accounts for 0.5% of hospital admissions for cardiovascular reasons.
Frequently affects young population of mainly male patients.
Endomyocardial biopsy in patients with unexplained cardiomyopathy 10 to 17% of patients have myocarditis.
Autopsy studies show myocarditis to be present in about 5% of individuals in unselected cases, but the disease is considered the main cause of death in only a minority of cases.
Process is underdiagnosed.
Nucleic acid test for community acquired respiratory viruses such as influenza should be performed.
Molecular and serologic test for cytomegalic virus, Epstein-Barr virus, parvovirus and HIV should be performed.
Less common types of infectious causes of myocarditis include Chagas’ disease, toxoplasmosis, Lyme disease, and trichinosis.
In infectious myocarditis a direct effect of the infectious agent or the resultant immune reaction can cause repolarization abnormalities in myocytes associated well associated foci of microabscesses or microaneurysmic arrhythmogenic foci.
Usually a transient and focal inflammation of the myocardium.
The prognosis of patients with acute myocarditis can be predicted on patient’s clinical presentation: patients with ventricular arrhythmias or reduced left ventricular ejection fraction as well as those with heart failure are prone to have the worse prognosis including a higher rate of short and long-term adverse outcomes compared to those presenting with normal cardiac function, without symptoms of heart failure and with no ventricular arrhythmias.
Myocarditis inflammation may involve the myocardium with involvement of the conduction system, leading to arrhythmias, including complete AV block.
There is a low in-hospital complication rate among patients with acute myocarditis.
Systolic dysfunction was the most powerful predictor of in-hospital adverse events.
The overall prognosis of patients with acute myocarditis is good.
Endomyocardial biopsy reserved for patients with rapidly progressive heart failure or arrhythmias in which a histological diagnosis is required before the initiation of immunosuppressive therapy.
Process ranges from subclinical, or benign form, to a major clinical syndrome such a severe heart failure or life-threatening ventricular arrhythmias.
Its presentation is variable, ranging from nonspecific fatigue and chest pain to heart failure, arrhythmia, or sudden death.
Causes include infections, immune mediated, and toxin mediated causes.
Myocarditis can be categorized as acute of three months or less of symptoms, or subacute, or chronic with symptoms greater than three months.
The main clinical manifestations of chest pain with an otherwise uncomplicated picture and no ventricular arrhythmias new or worsening heart failure, chronic heart failure, life-threatening hemodynamic compromise, life-threatening arrhythmias or conduction disturbances.
Most cases three main patterns of presentation: recent onset of heart failure of less than six months duration, arrhythmias, and chest pain.
Approximately 82 to 95% of patients report chest pain, 19 to 49% report dyspnea, 58-65% develop fever and 5 to 7% experience syncope.
Cardiogenic shock occurs in about 3 to 9% of patients with acute myocarditis.
Clinical presentation can predict the outcome with patients having reduced LVEF, heart failure, advanced AV block, sustained ventricular arrhythmias, or cardiogenic shock, are at an increased risk for death or heart transplantation.
Most patients have an uncomplicated course, with chest pain in 97% of patients and ST segment elevation on EKG in 62%, with no deaths or transplantation at five years.
High sensitivity troponin I or T levels are elevated in approximately 64 to 100% of patients.
C reactive protein level is elevated in approximately 54 to 99% of patients.
Heart transplantation or death from cardiac causes occurs almost exclusively in patients who present with acute myocarditis and left ventricular ejection fraction of less than 50%, sustained ventricular arrhythmias, hemodynamic instability or a combination of these.
Giant cell myocarditis carries the highest risk and should be suspected in patients with rapidly progressive heart failure or cardiogenic shock that does not respond to usual therapy.
Clinical suspicion should arise with the above criteria and when the major contribution of other diseases such as coronary heart disease, valvular heart disease, congenital heart disease, or hypertensive cardiomyopathy has been excluded.
Diagnostic testing includes a complete CBC, measurement of acute phase reactants and cardiac biomarkers, chest x-ray, electro cardiography, and echocardiography.
Echocardiogram changes or consistent with myocardial increased wall thickness and abnormal myocardial echogenicity.
There may be mild segmental involving the inferior and lateral walls, diastolic dysfunction, and pericardial effusion.
Left ventricular ejection fraction is preserved in approximately 75% of patients, however, cardiac functions may decline rapidly during the initial days after presentation.
Endomyocardial biopsy is reserved for patients with clinically suspected myocarditis with cardiogenic shock or acute heart failure requiring inotropic or mechanical circulatory support, ventricular arrhythmias, Mobitz type II second-degree or higher AV block, particularly when symptom onset is recent, with mild to no left ventricular dilatation, peripheral eosinophilia or associated systemic inflammatory disorder, persistent a recurrent release in necrosis markers, particularly when an autoimmune condition is likely or ventricular rhythm and high degree AV block are present or cardiac dysfunction in a patient receiving immune checkpoint inhibitor therapy.
Cardiac MRI should be considered as the initial diagnostic test to detect inflammation, and endocardial biopsy may be considered on that basis.
Cardiac MRI in cases of clinically suspected myocarditis should be performed within 2 to 3 weeks after initial presentation and is useful for its diagnostic sensitivity and for assessment and follow up to monitor the evolution of the disease.
MRI findings include intense gadolinium enhancement, indicating hyperemia, increased myocardial T2 relaxation time reflecting tissue edema, and late gadolinium enhancement indicating necrosis or fibrosis.
MRI findings also help in risk stratification identifying patients with favorable or unfavorable outcomes depending upon the persistence of gadolinium and edema.
Endomyocardial biopsy reveals an inflammatory infiltrate, with necrosis or degeneration of adjacent monocytes.
Subtypes such as lymphocytic, eosinophilic, and giant cell myocarditis and sarcoidosis have specific prognostic and therapy implications.
The presence of fibrosis should be evaluated.
The diagnostic yield of endomyocardial biopsy is highest in the first two weeks after onset of symptoms.
Markers of myocyte injury, and inflammation include the ESR and C reactive protein levels: although they are not specific, and not necessarily increased in myocarditis.
Troponin is a more sensitive marker than creatine kinase, but an elevated creatine kinase level could suggest the association of myocarditis with skeletal myositis.
A high sensitivity, troponin assay can detect myocarditis more accurately then a conventional troponin test.
Brain, natriuretic peptides can be useful, but are nonspecific and normal results do not rule out myocarditis.
Screening for autoimmune disease is recommended in patients with suspected myocarditis.
TREATMENT:
Treatment is based on the acuity, severity ideology, and clinical presentation.
Patients are characterized into complicated or uncomplicated forms of myocarditis with presence of left ventricular systolic function, heart failure, ventricular, arrhythmias, or advanced, atrioventricular conduction disturbances, or cardiogenic shock.
Because myocarditis can be a reversible disease, the main goals of treatment are biventricular unloading, adequate systemic and coronary perfusion, and venous decongestion to prevent multiorgan dysfunction, provide a bridge to recovery, transplantation, or use of a durable assist device.
Management of arrhythmias and heart failure are goals of treatment.
Patients with uncomplicated myocarditis can be treated with non-steroidal anti-inflammatory drugs, including aspirin to relieve chest pain.
Acute myocarditis associated with systemic auto immune disorders is generally treated with corticosteroids as first line treatments: Higher doses or additional immunosuppressive therapies are reserved for patients with complicated presentation.
Immune checkpoint inhibitor associated acute myocarditis is treated by stopping the immune checkpointinhibit therapy and initiating high dose intravenous corticosteroids.
Giant cell myocarditis is treated with immunosuppression, including anti-thymocyye and cyclosporine blocking T cell infiltration of myocardium and is also combined with high dose intravenous corticosteroids.
Acute myocarditis due to sarcoidosis is typically treated with corticosteroids with methotrexate as the second line therapy as well as azathioprine and anti-tumor necrosis factor inhibitors.
Myocarditis with eosinophilic infiltrates is generally treated with corticosteroids.
Treatment with beta blockers is associated with better outcomes, but evidence is poor.
Hemodynamically stable heart failure is treated with diuretics, ACE inhibitors/angiotensin receptor blockade and beta adrenergic blockade:aldosterone may be added in patients with persistent heart failure.
Patients with unstable hemodynamics and heart failure require inotropic agents in an intensive care unit with respiratory and mechanical cardiopulmonary support.
Patients with cardiogenic shock with severe ventricular dysfunction may require mechanical circulatory support with ventricular assist devices or extracorporeal membrane oxygenation.
Arrhythmic management follows guidelines and may include pacing and defibrillator implants.
Immunosuppressive drugs are therapies for eosinophilic myocarditis, and for giant cell, myocarditis and cardiac sarcoidosis.
No specific therapies available for lymphocytic acute myocarditis, except for forms associated with systemic diseases and immune checkpoint inhibitors.
Heart failure therapies with ACE inhibitors, beta blockers, mineralcorticoid receptor, antagonists, and and angiotensin receptor – neprilyssin inhibitors, and sodium glucose co transporter 2 inhibitors are recommended with reduced LVEF and stable hemodynamics.
With severe left ventricular systolic dysfunction inotropic agents such as norepinephrine, epinephrine, or milrinone, are required, or temporary mechanical circulatory supports such as intraaortic baloon pump, venoarterial extracorporal membrane oxygenator, or intra-aortic axial pumps are required.
In patients where temporary, mechanical circulatory support cannot be removed, urgent heart transplant may be considered.
Evidence supporting treatment of acute myocarditis with corticosteroids is lacking.
The incidence of sudden cardiac death related to acute myocarditis in younger adults is approximately 6 to 10% and an implantable cardioverter-defibrillator may be considered in patients at high risk for ventricular arrhythmia after myocarditis.
