B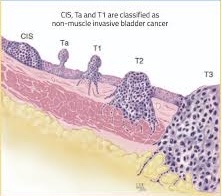 Muscle-invasive bladder cancer (MIBC) refers to a stage of bladder cancer where the tumor has penetrated into the muscularis propria of the bladder wall.
Muscle-invasive bladder cancer (MIBC) refers to a stage of bladder cancer where the tumor has penetrated into the muscularis propria of the bladder wall.
This stage is classified as T2 or higher in the TNM staging system.
MIBC is associated with a higher risk of metastasis and poorer prognosis compared to non-muscle-invasive bladder cancer (NMIBC).
MIBC increases the risk for distant spread, with common metastatic sites including lymph nodes, bone, lung, liver, and peritoneum.
Micrometastatic disease occurs enough to 50% of muscle invasive bladder cancers.
Approximately 50% of patients with muscle invasive bladder cancer have recurrence within three years.
Bladder cancer is the third most common cancer in men, with more than 83,000 new cases diagnosed in men and women.
About 25% of bladder cancers are MIBCs.
Neoadjuvant chemotherapy to debulk, existing tumors and micrometastases is the current standard of care.
The use of immunotherapy in the setting of MIBC suggest that treatment will activate systemic T cell response to tumor antigens, enhancing the detection and killing a micrometastatic disease.
Smoking tobacco may be the cause of half of all bladder tumors.
Contact with chemicals used to make plastics, paints, textiles, leather and rubber may cause bladder cancer.
Ta: Tumor on the bladder lining that does not enter the muscle Tis: Carcinoma in situ – a high-grade cancer – looks like a reddish, velvety patch on the bladder lining T1: Tumor goes through the bladder lining but does not reach the muscle layer T2: Tumor grows into the muscle layer of the bladder T3: Tumor goes past the muscle layer into tissues around the bladder T4: Tumor has spread to nearby structures such as lymph nodes and the prostate in men or the vagina in females.
MIBC is when the cancer has grown far into the wall of the bladder (Stages T2 and beyond).
For patients with MIBC, the overall prognosis is dependent on stage and treatment.
In patients who have a cystectomy the cancer return rate can be from 20-30% for stage T2.
The cancer return rate can be 40% for T3, greater than 50% for T4 and often higher when lymph nodes are involved.
If bladder cancer does come back, it most often will happen within the first two years after bladder surgery.
Treatments for muscle invasive bladder cancer include:
Bladder removal (cystectomy) with chemotherapy or without chemotherapy
Chemotherapy with radiation, in addition to TURBT
For MIBC, chemotherapy is likely to be given before radical cystectomy.
Bladder removal with chemotherapy raises survival rates for bladder cancer patients.
Neoadjuvant chemotherapy should include the drug cisplatin.
Chemotherapy given before bladder removal is best survival rates.
For MIBC,the whole bladder is removed.
When the bladder is removed, a pelvic lymph node dissection is standard of care.
There are many things to think about before choosing open or robotic bladder removal.
For MIBC, the most common type of surgery is radical cystectomy.
The surgeon removes the whole bladder, nearby lymph nodes and part of the urethra.
In men, the surgeon also may remove the prostate.
In females, the surgeon may remove the uterus, fallopian tubes, ovaries and vaginal wall.
When the whole bladder is removed, a urinary diversion is performed.
Partial cystectomy may be considered cancer in which tumor is found in a specific part of the bladder.
Urinary diversion choices:
Ileal conduit:
Continent cutaneous reservoir:
Orthotopic neobladder:
Chemotherapy with radiation may be used for bladder preservation keeping the bladder or parts of it.
Bladder preservation may be suggested for select patients where radical cystectomy is not an option or is undesired.
Radiation alone for MIBC is not a choice to control the spread of bladder tumors.
Some chemotherapy drugs that may be used along with radiation are cisplatin, 5-FU and Mitomycin-C.
For patients who use the multi-modal approach to bladder preservation, 30% of the time MIBC will return.
Imaging (e.g. CT scan) about every 3-6 months for 2-3 years; and then once a year.
Laboratory tests may be every 3-6 months for 2-3 years; and then once a year.
Guidelines recommend radical cystectomy with neoadjuvant cisplatin-based chemotherapy as the standard treatment for MIBC, given its potential to improve survival outcomes.
For patients ineligible for cisplatin, alternative treatments such as trimodal therapy (TMT) combining transurethral resection, chemotherapy, and radiation are considered.
Among patients with high risk muscle invasive urothelial carcinoma after radical surgery, disease free survival is significantly longer with adjuvant Pembrolizumab than observation (Apolo AB).
A phase 3 randomized trial NIAGARA found the efficacy of neoadjuvant durvalumab a PD-L1 inhibitor plus gemcitabine-cisplatinum followed by radical cystectomy and adjuvant durvalumab every four weeks for eight cycles as compared with neoadjuvant gemcitabine, cisplatinum followed by radical cystectomy alone, in patients with muscle invasive bladder cancer showed the pathological complete response and event free survival, disease recurrence and death were improved.
