 Middle cerebral artery stroke describes the sudden onset of a focal neurologic deficit resulting from hemorrhagic or ischemic disruption of the middle cerebral artery’s blood supply.
Middle cerebral artery stroke describes the sudden onset of a focal neurologic deficit resulting from hemorrhagic or ischemic disruption of the middle cerebral artery’s blood supply.
The MCA is by far the largest cerebral artery and is the vessel most commonly affected by cerebrovascular accident (CVA).
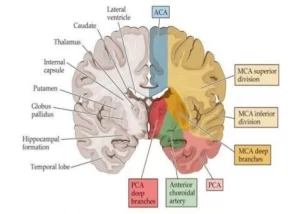
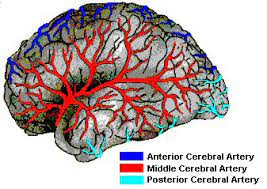
The MCA supplies most of the outer convex brain surface, nearly all the basal ganglia, and the posterior and anterior internal capsules.
Infarcts that occur within the large distribution of this vessel lead to diverse neurologic sequelae.
Large space occupying middle cerebral artery or hemispheric ischemic brain infarcts are associated with massive brain edema which may lead to brain herniation and early demise.
The massive middle cerebral artery infarction, described as malignant middle cerebral artery infarction, is associated with a 80% mortality due to brain herniation during the first week after the event.
Present therapy including osmotherapy, hyperventilation, and barbiturates are inadequate measures.
A decompressive hemicraniectomy which involves temporary removal of a large part of the skull, combined with a duraplasty allows edematous tissue to expand outside the neurocranium, preventing fatal internal displacement of brain tissue and subsequent herniation (Huttner H, Schwab S).
Randomized controlled trials have shown the benefit of early hemicraniectomy, within 48 hours after the onset of stroke, increased from survival from 29% to 78%.
The survival rate with severe disability is only 4-5%.
43% of patients who underwent hemicraniectomy have a relatively good outcome compared to 21% for patients with conservative therapy (Vahedi K et al).
The benefit of such surgery in older patients is uncertain.
A randomized controlled study of patients 61 years of age or older with malignant middle cerebral artery infarction to either conservative therapy or hemicraniectomy made within 48 hours after the onset of symptoms: The proportion of patients who survived without severe disability was 38% in the hemicraniectomy group, compared to 18% in the control group (DESTINY II Investigators).
In the above study lower mortality in the surgical group was 33% versus 70% in the conservative therapy group.
Most patients that survived had substantial disability.
