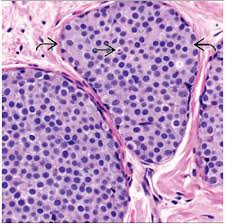
 Proliferation of homogenous malignant cells within the terminal duct lobular apparatus.
Proliferation of homogenous malignant cells within the terminal duct lobular apparatus.
Along with atypical lobular hyperplasia represents a breast disease referred to as lobular neoplasia.
5% of all breast cancer specimens contain LCIS.
Highest incidence rate of 11.4 100,000 person-years occurs in women age 50-59 years.
High rate of multicentricity and multifocality.
Marker for increased risk of breast cancer.
Most women with LCIS will not develop breast cancer in her lifetime.
Lifetime risk of breast cancer may exceed 20%.
Associated with an 8-10 fold increase of risk breast cancer.
The probability of developing cancer or invasive type is 13% in the first 10 years after diagnosis, 26% after 20 years 35% by 35 years, or approximately 1% a year (Bodian CA et al).
Associated with calcifications on mammograms and 21-67% of cases (Li CI et al).
With pure LCIS the risk of developing invasive carcinoma is about 21% over 15 years (Haagensen CD et al).
Women with diagnosed DCIS or LCIS have an approximately 4 times risk of developing invasive breast cancer than the general population (Warnberg).
Transforms into invasive carcinoma at a very low rate.
Risk of invasive carcinoma after a diagnosis of lobular neoplasia is equal in both breasts.
An invasive cancer that may eventually develop is equally likely to be a ductal as a lobular lesion.
Criteria for pathologic diagnosis includes characteristic and uniform cells rising the entire population of cells within the lobular unit, all of the lobule must be filled with his cells, there must be distention and extension of at least half of the acini in the lobular unit.
Diagnosis following surgical excision does not require further surgical management and there is no need to document margins status if only lobular neoplasia is present in the biopsy.
The findings of LCIS in surrounding breast parenchyma of a lumpectomy specimen containing DCIS or invasive breast cancer does not alter the management of the primary breast tumor, and does not increase the rate of recurrence in patients undergoing breast conservation.
When identified on core needle biopsy diagnosis of LCIS should be followed by a surgical excision of the lesion to rule out an associated breast cancer.
Following a surgical excision of a core biopsy with LCIS, approximately 1/3 of patients will be upstaged to either DCIS or invasive cancer, although a recent study suggests upstaging is much less frequent and routine excision may not be warranted (Translational Breast Research Cancer Consortium). Risk reduction mastectomy is an option for such patients.
Typically an incidental finding and a breast biopsy on for another reason.
Has no specific clinical or radiographic features, therefore it is mostly clinically occult.
When clinically identified by physical exam or mammography is frequently multicentric and bilateral.
Usually recognized as an incidental finding at the time of breast biopsy for another lesion, therefore true incidence is unknown.
Fourfold increase in incidence in last three decades, specifically in postmenopausal women and corresponds to the similar increase of infiltrating lobular carcinoma among women 50 years or older.
Following diagnosis surveillance is the minimum action necessary: including clinical breast exam every 6-12 months and annual mammography.
MRI screening is not presently supported by data.
Tamoxifen in the National Surgical Adjuvant Breast Project Breast Cancer Prevention Trial given for 5 years in LCIS reduced the risk of developing invasive breast cancerby approximately 46%.
Raloxifene and Tamoxifen in the NSABP Study of Tamoxifen and Raloxifene (STAR trial) were equally effective in reducing the risk of invasive cancer in postmenopausal women with LCIS.
