
 Refers to endoscopy of the larynx.
Refers to endoscopy of the larynx.
It is a medical procedure that is used to obtain views, of the vocal folds and the glottis.
May facilitate tracheal intubation or cardiopulmonary resuscitation or for surgical procedures on the larynx or other parts of the upper tracheobronchial tree.
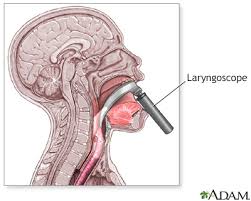
Direct laryngoscopy is carried out with the patient lying on his or her back.
The laryngoscope is inserted into the mouth and move the tongue out of the line of sight.
It is inserted either anterior or posterior to the epiglottis and then lifted with an upwards and forward motion, allowing a view of the glottis.
The procedure is done with full preparation for resuscitative measures to deal with respiratory distress.
There are at least ten different types of laryngoscope used for this procedure.
It is most often used by anaesthetists for endotracheal intubation under general anaesthesia
The procedure can be used for diagnostic laryngoscopy with biopsy.
It is not typically performed on conscious patients, or on patients with an intact gag reflex.
In indirect laryngoscopy the vocal cords are visualized by a means other than obtaining a direct line of sight as with a mirror.
Laryngoscopy aids in intubation during the administration of general anesthesia or for mechanical ventilation.
Laryngoscopy helps detect causes of voice changes, causes of throat and ear pain, evaluates difficulty in swallowing, detects strictures or injury to the throat, or obstructive masses in the airway.
The vast majority of tracheal intubations involve the use of a laryngoscope.
The conventional laryngoscope consists of a handle containing batteries with a light source, and a set of interchangeable blades.
Early laryngoscopes used a straight blade.
Two basic styles of laryngoscope blade are currently available: the curved blade and the straight blade.
The Macintosh blade is the most widely used of the curved blades.
The Miller blade is the most popular style of straight blade.
Both types blades are available in sizes 0 (neonatal) through 4 (large adult).
Other styles of curved and straight blades with accessories such as mirrors for enlarging the field of view and even ports for the administration of oxygen designed for use by anesthetists.
Paramedics are trained to use direct laryngoscopy.
The Macintosh blade is positioned in the vallecula, anterior to the epiglottis, lifting it out of the visual pathway.
The Miller blade is positioned posterior to the epiglottis, trapping it while exposing the glottis and vocal folds.
Incorrect usage can cause trauma to the front incisors.
The Miller, Wisconsin, Wis-Hipple, and Robertshaw blades are commonly used for infants, as it is easier to visualize the glottis using these blades than the Macintosh blade in infants, due to the larger size of the epiglottis relative to that of the glottis.
The conventional direct laryngoscope uses a line of sight provided by a rigid viewing instrument with a light on the blade or intra-oral portion which requires a direct view of the target larynx.
The conventional direct laryngoscope provides a direct view in 80-90% of attempts, so failures of direct laryngoscopy led to the development of alternative devices such as the lighted stylet, and a number of indirect fiberoptic viewing laryngoscopes, such as the fiberscope, Bullard scope, Upsher scope, and the WuScope.
A video laryngeal scope includes the same components as those of a direct laryngoscope but it’s also equipped with the camera positioned in the distal half of the blade that transmits images to a screen.
With the aid of the video screen to visualize the vocal cords, guiding the endotracheal tube can be done through vocal cords without a direct line of sight from the mouth.
Among critically ill adults undergoing tracheal intubation in an emergency setting the use of video laryngoscope resulted in a higher incidence of successful intubation on the first attempt, than the use of direct laryngoscope (Pragmatic critical care research group).
Among neonates undergoing urgent endotracheal intubation, video laryngoscopy, resulted in the greater number of successful intubations on the first attempt than direct laryngoscopy.
Injury caused by use of laryngoscopes include: minor damage to the soft tissues within the throat, sore throat,major injuries to the larynx and pharynx causing permanent scarring, ulceration, abscesses, and a risk of causing tooth damage.
