 Pancreatic islets are groups of cells found within the pancreas that release hormones.
Pancreatic islets are groups of cells found within the pancreas that release hormones.
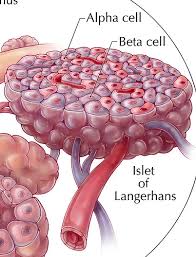
Also known as Islets of Langerhans.
The pancreatic islets or islets of Langerhans are the regions of the pancreas that contain its endocrine cells.
The pancreatic islets constitute 1–3% of the pancreas volume and receive 10–15% of its blood flow.
The pancreas has approximately 1 million islets.
Islets weigh 1-1.5 gm.
Most measure 100-200 µm and consist of four major and two minor cell types.
Five types ß, α, δ, e and PP (pancreatic polypeptide) cells, making 68%, 20%, 10% and 2%, respectively of the islet cell population.
The pancreatic islets are arranged in density routes throughout the human pancreas, and are important in the metabolism of glucose.
There are about 1 million islets distributed throughout the pancreas of a healthy adult human, each of which measures an average of about 0.2 mm in diameter.
Each islet is separated from the surrounding pancreatic tissue by fibrous connective tissue capsule which is continuous with the fibrous connective tissue that is interwoven throughout the rest of the pancreas.
Hormones produced in the pancreatic islets are secreted directly into the blood by, at least, five types of cells.
Alpha cell secrete glucagon, beta cells secrete insulin, delta cells secrete somatostatin, epsilon secrete ghrelin, and PP cells secrete pancreatic polypeptide.
Alpha cells producing glucagon are 20% of total islet cells.
Beta cells producing insulin and amylin, about 70%.
The proportion of beta cells in islets it is about 40–50%.
PP cells (gamma cells or F cells) producing pancreatic polypeptide. Less than 5%.
Delta cells producing somatostatin <10%.
Epsilon cells producing gherkin <1%.
Islets display alpha and beta cells in close relationship with each other throughout the cluster.
In addition to endocrine cells, there are stromal cells (fibroblasts), vascular cells (endothelial cells, pericytes), immune cells (granulocytes, lymphocytes, macrophages, dendritic cells) and neural cells in the islets.
A large amount of blood flows through the islets, 5–6 mL/min per 1 g of islet.
Blood flow in the islets is up to 15 times more than in exocrine tissue of the pancreas.
The hormones are released in a balanced mixture into the portal vein in reaction to changes in the plasma levels.
The majority of the endocrine cells are located in the islet cell periphery, while the beta cells are located in the center and comprise 70% of the islet mass.
Alpha cells are predominantly seen in the islet cells in the superior aspect of the pancreatic head, body, and tail; it accounts for 10% of the islet mass.
Delta cells are like beta cells, which are present in all islets throughout the pancreas.
Delta cells make up only 5% of the islet cell mass.
PP cells are mostly seen in the islets in the pancreas’ head and account for 15% of the islet mass.
Islets can influence each other through paracrine and autocrine communication, and beta cells are coupled electrically to six to seven other beta cells, but not to other cell types.
Glucose/Insulin: activates beta cells and inhibits alpha cells.
Glycogen/Glucagon: activates alpha cells which activates beta cells and delta cells.
Somatostatin: inhibits alpha cells and beta cells, and also inhibits the secretion of pancreatic polypeptide.
A large number of G protein-coupled receptors (GPCRs) regulate the secretion of insulin, glucagon and somatostatin from pancreatic islets,and some of these GPCRs are the targets of drugs used to treat type-2 diabetes (GLP-1 receptor agonists, DPPIV inhibitors).
The beta cells of the pancreatic islets secrete insulin.
It is thought that they are destroyed by immune assaults.
Insulin independence and improved metabolic control can be reproducibly obtained after transplantation of cadaveric donor islets into patients with unstable type 1 diabetes.
People with high body mass index (BMI) are unsuitable pancreatic donors due to greater technical complications during transplantation.
However, it is possible to isolate a larger number of islets because of their larger pancreas, and therefore they are more suitable donors of islets.
Islet transplantation only involves the transfer of tissue consisting of beta cells that are necessary as a treatment of this disease.
Islet transplantation represents an advantage over whole pancreas transplantation, which is more technically demanding and poses a risk of, for example, pancreatitis leading to organ loss, and does not require general anesthesia.
Islet transplantation for type 1 diabetes currently requires potent immunosuppression to prevent host rejection of donor islets.
There is a risk of portal venous branch thrombosis and the low value of islet survival a few minutes after transplantation.
Neovascularization is key to islet survival, supported by VEGF produced by islets and vascular endothelial cells.
