 Refers to newborn bleeding into the ventricles of the brain.
Refers to newborn bleeding into the ventricles of the brain.
Most often seen in premature infants born before 30 weeks of pregnancy.
The smaller and more premature the infant, the higher the risk of such bleeding because blood vessels in the brain of premature infants are not fully developed and are extremely fragile.
More common in premature babies who have had respiratory distress syndrome and hypertension.
May also occur in healthy premature babies who were born without injury and very rarely in full-term infants.
Usually occurs in the first several days of life, and a rare event after 1 month of age.
The site of origin of IVH is the subependymal germinal matrix, a region of the developing brain associated with neuronal proliferation that is completed by 20 weeks gestation.
In the subependymal germinal matrix neuronal proliferation occurs as neuroblasts divide and migrate into the cerebral parenchyma.
Cells of the germinal matrix have significant numbers of mitochondria and are sensitive to ischemia.
Autoregulation, the ability to regulate cerebral blood flow, is frequently compromised in very premature infants with pulmonary disease and may be related to the development of IVH.
Suppressing the respiratory efforts of the neonate with respiratory distress by pharmacological muscle blockade reduces the risk of IVH.
The major complication of IVH relates to the damage to cerebral parenchyma and the development of posthemorrhagic hydrocephalus.
Parenchymal hemorrhages the development of necrotic areas form cysts that can become contiguous with the ventricles and ref2242ed to as porencephalic cysts.
Cerebral palsy is the primary neurological disorder observed after periventricular-IVH, although mental retardation and seizures can ensue as well.
Long-term neurological outcome can also be altered is through the development of posthemorrhagic hydrocephalus.
At present, based upon conflicting results of large multicenter trials discussed above, the long-term benefit of indomethacin prophylaxis for IVH in preterm infants is still debatable.
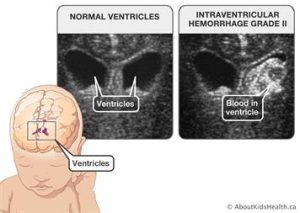
Classified by four grades: based on radiological appearance.
Grade I hemorrhage minimal or grade I periventricular hemorrhage.
Grade II – Subependymal hemorrhage with extension into lateral ventricles without ventricular enlargement.
Grade III – Subependymal hemorrhage with extension into lateral ventricles with ventricular enlargement.
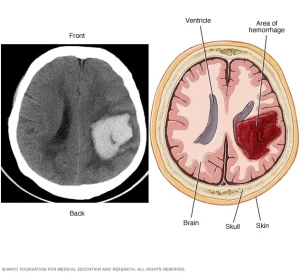
Grade IV – Intraparenchymal hemorrhage
Blood clots that form in the ventricular system can block the flow of cerebrospinal fluid, leading to hydrocephalus.
Process may be asymptomatic or include: apnea, alterations in blood pressure, heart rate, decreased muscle tone, decreased relexia, lethargy, sleepiness, and weak sucking reflex.
Ultrasound of the head is recommended for all babies before 30 weeks to screen for IVH and is performed once between 7 and 14 days of age.
CT scan of the head is recommended with a difficult birth, low blood count, or signs of bleeding problems.
Treatment is symptomatic.
A spinal tap or a ventriculostomy or intraventricuar shunt may be done to relieve intracranial pressure.
Severe intraventricular bleeding may lead to developmental delays and problems controlling movement.
Intrapartum corticosteroids may reduce risk for IVH.
Complications of periventricular-IVH include life-long neurological deficits, such as cerebral palsy, developmental delay, and seizures.
