 Intraventricular hemorrhage (IVH), also known as intraventricular bleeding, is a bleeding into the brain’s ventricular system.
Intraventricular hemorrhage (IVH), also known as intraventricular bleeding, is a bleeding into the brain’s ventricular system.
The intraventricular system is where the cerebrospinal fluid is produced and circulates through towards the subarachnoid space.
It can result from physical trauma or from hemorrhagic stroke.
30% of intraventricular hemorrhage (IVH) are primary, confined to the ventricular system and typically caused by intraventricular trauma, aneurysm, vascular malformations, or tumors, particularly of the choroid plexus.
However 70% of IVH are secondary to an expansion of an existing intraparenchymal or subarachnoid hemorrhage.
Intraventricular hemorrhage has been found to occur in 35% of moderate to severe traumatic brain injuries.
Symptoms of IVH are similar to other intracerebral hemorrhages and include sudden onset of headache, nausea and vomiting, together with an alteration of the mental state and/or level of consciousness.
Focal neurological signs are either minimal or absent.
Focal and/or generalized seizures may occur with intraventricle hemorrhage.
Xanthochromia in CSF is the rule.
Some infants with intraventricular bleed are asymptomatic and others may present with hard to detect abnormalities of consciousness, muscle tone, breathing, movements of their eyes, and body movements.
Causes of IVH in adults include physical trauma or from hemorrhagic stroke.
Infants that are preterm and very low birth weight are also at high risk for INH.
IVH has been reported to occur in approximately 25% of infants who are born with a very low birth weight.
Approximately 12,000 infants each year are diagnosed with germinal matrix hemorrhage or intraventricular hemorrhage in the United States.
IVH in the preterm brain usually arises from the germinal matrix whereas IVH in the term infants originates from the choroid plexus.
IVH it is common in premature infants or those of very low birth weight.
The cause of IVH in premature infants is rarely due to trauma.
In preterm infants, intraventricular hemorrhage and germinal matrix haemorrhage are the most widely reported neurological disorders.
IVH in premature infants is thought to result from changes in perfusion of the delicate cellular structures in the growing brain, augmented by the immaturity of the cerebral circulatory system, which is especially vulnerable to hypoxic ischemic encephalopathy.
When a lack of blood flow results, cell death and subsequent breakdown of the blood vessel walls, lead to bleeding.
Most intraventricular hemorrhages occur in the first 72 hours after birth.
The risk is increased with use of extracorporeal membrane oxygenation in preterm infants.
Congenital cytomegalovirus infection can be an important cause of IVH.
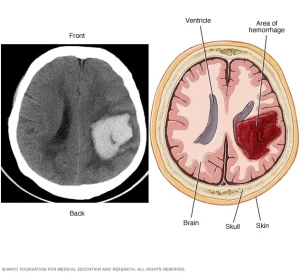
Diagnosis is confirmed by the presence of blood inside the ventricles on CT.
In term and preterm infants with IVH it is often described in four grades:
Grade I – bleeding occurs just in the germinal matrix
Grade II – bleeding also occurs inside the ventricles, but they are not enlarged
Grade III – ventricles are enlarged by the accumulated blood
Grade IV – bleeding extends into the brain tissue around the ventricles
Grades I and II are most common, and often there are no further complications.
Grades III and IV are the most serious and may result in long-term brain injury to the infant.
After a grade III or IV IVH, blood clots may form which can block the flow of cerebrospinal fluid, leading to hydrocephalus.
Head positioning in very preterm infants has been suggested as an approach to prevent germinal matrix hemorrhage.’
Approaches include bed tilting, supine mid-line head positioning, supine head rotation 90 degrees, prone mid-line head positioning, head tiling.
Interventions are based on clinical signs and symptoms of ventricular dilatation.
Attention is placed on intracranial pressure (ICP) monitoring via an intraventricular catheter and medications to maintain ICP, blood pressure, and coagulation.
In more severe cases an external ventricular drain may be required to maintain ICP and evacuate the hemorrhage, and in extreme cases an open craniotomy may be required.
In infants therapies employed into preventing the high rates of morbidity and mortality, including diuretic therapy, repeated lumbar puncture, streptokinase therapy and a combination of drainage, irrigation and fibrinolytic therapies.
In infants, germinal matrix hemorrhage is associated with cerebral palsy, problems with cognition, and hydrocephalus.
With improved technological advances survival for preterm infants with this type of neurological disorder has improved and less preterm infants with germinal matrix hemorrhage have severe cerebral palsy.
An estimated 15% of preterm infants who survive develop cerebral palsy and 27% of the infants who survive experience moderate to severe neurosensory deficits by the time they reach 18–24 months old.
Prognosis is very poor when IVH results from intracerebral hemorrhage is related to high blood pressure
Prognosis is very poor when IVH results when hydrocephalus follows.
IVH can result in increases in ICP and can cause potentially fatal brain herniation.
Intraventricular blood clotting can lead to blocking of CSF flow and to obstructive hydrocephalus which may quickly result in increased intracranial pressure and death.
Breakdown products from the blood clot may generate an inflammatory response damagING the arachnoid granulations, inhibiting the regular reabsorption of CSF and resulting in permanent communicating hydrocephalus.
Traumatic brain contusions and subarachnoid hemorrhages are commonly associated with IVH.
The IV bleeding can involve the anterior communicating artery or the posterior communicating artery.
