
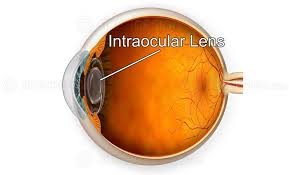
 An Intraocular lens (IOL) is a lens implanted in the eye usually as part of a treatment for cataracts or for correcting other vision problems such as short sightedness and long sightedness.
An Intraocular lens (IOL) is a lens implanted in the eye usually as part of a treatment for cataracts or for correcting other vision problems such as short sightedness and long sightedness.
An intraocular lens (IOL) is a synthetic lens that is implanted inside the eye during cataract surgery to replace the natural crystalline lens of the eye after it has been removed.
The main purpose is to restore clear vision after the natural lens has become clouded by a cataract, and the IOL provides the refractive power necessary for focusing light onto the retina.
Different types of IOL’s include monofocal IOLs which are fixed single focus, multifocal IOLs that provide distance and near vision, toric IOLs that correct astigmatism, and accommodating IOLs that attempt to mimic the eye’s natural focusing ability.
IOLs are made of biocompatible plastic or silicone materials.
Implantation during cataract surgery the clouded natural lens is removed and the IOL is implanted and positioned into the evacuated capsular bag where the natural lens used to reside.
IOLs come in different diopter powers to correct the patient’s refractive error and focus light properly after lens removal.
Restoring clear vision, reducing dependence on glasses/contacts for distance vision, potential for correcting other refractive errors like astigmatism.
Placement if IOL’s is a form of refractive surgery.
If the natural lens is left in the eye, the IOL is known as phakic, otherwise it is a pseudophakic lens.
IOLs are designed to provide the same light-focusing function as the natural crystalline lens.
This can be an alternative to LASIK, but LASIK is not an alternative to an IOL for treatment of cataracts.
IOLs usually consist of a small plastic lens with plastic side struts, called haptics.
The haptics hold the lens in place in the capsular bag inside the eye.
Most IOLs fitted today are fixed monofocal lenses matched to distance vision, but other types are available, such as a multifocal intraocular lens that provides multiple-focused vision at far and reading distance, and adaptive IOLs that provide limited visual accommodation.
Multifocal IOLs can also be Trifocal IOLs or extended depth of focus lenses.
Nearly 28 million cataract procedures take place annually worldwide.
There are about 75,000 procedures per day globally.
The procedure is usually done under local or topical anesthesia with the patient awake throughout the operation.
The use of a flexible IOL enables the lens to be rolled for insertion into the capsular bag through a very small incision, thus avoiding the need for stitches.
This procedure usually takes less than 30 minutes, and the recovery period is about 2–3 weeks.
Following surgery avoiding strenuous exercise or anything else that significantly increases blood pressure is recommended.
IOL implantation risks associated with eye surgeries: infection, loosening of the lens, lens rotation, inflammation, nighttime halos and retinal detachment.
IOLs enable many patients to have reduced dependence on glasses, yet, most patients still rely on glasses for certain activities, such as reading.
These reading glasses may be avoided if multifocal IOLs, trifocal IOLs or extended depth of locus lenses are used.
Intraocular lenses for correcting larger errors in near-sighted, far-sighted, and astigmatic eyes, also called phakic intraocular lens, as it is implanted without removing the patient’s natural crystalline lens.
Phakic IOL appear to be lower risk than excimer laser surgery (LASIK) in those with significant nearsightedness.
More commonly, IOLs are implanted via Clear Lens Extraction And Replacement (CLEAR) surgery.
During CLEAR, the crystalline lens is extracted and an IOL replaces it in a process that is very similar to cataract surgery: both involve lens replacement, local anesthesia, last approximately 30 minutes, and require making a small incision in the eye for lens insertion.
People recover from CLEAR surgery 1–7 days after the operation, avoiding strenuous exercise or anything else that significantly raises blood pressure.
CLEAR has a 90% success rate.
Risks of CLEAR surgery include wound leakage, infection, inflammation, and astigmatism.
CLEAR can be performed only on patients ages 40 and older to ensure that eye growth, which disrupts IOL lenses, will not occur post-surgery.
IOLs have three major benefits: an alternative to the excimer laser procedure (LASIK), eliminate the need for glasses or contact lenses post-surgery for most patients, and the cataract will not return.
The disadvantage is that the eye’s ability to change focus has been reduced or eliminated, depending on the kind of lens implanted.
Some of the risks found so far during a three-year study include:
a yearly loss of 1.8% of the endothelial cells,
0.6% risk of retinal detachment,
0.4% risk of corneal swelling
0.03–0.05% eye infection risk, which in worst case can lead to blindness.
glaucoma,
astigmatism,
remaining near or far sightedness,
rotation of the lens inside the eye one or two days after surgery.
Unsatisfactory refractory correction is that the lens may be incorrectly placed by the surgeon, or rotate inside the eye if is too short.
When standard IOLs are implanted with a CLEAR procedure, astigmatism is typically not corrected, as astigmatism is mainly attributable to a deformation of the cornea.
Toric IOLs may be used during the CLEAR procedure to correct astigmatism.
Indications for refractive lens exchange (RLE) include severe myopia or hyperopia with coexisting presbyopia as the primary indicators for RLE, as RLE leads to complete loss of accommodation.
Underlying regular astigmatism can also be managed by RLE.
Complications of RLE are similar to those after cataract surgery.
RLE is often used in very short or very long eyes and patients’ ages tend to be significantly lower, so consideration must be given to longer term effects.
Implants can be used with or without removal of the natural crystalline lens:
Phakia is the presence of the natural crystalline lenses.
Phakic IOL (PIOL) refers to an intraocular lens implanted without removal of the original crystalline lens, and this is performed solely to correct refractive error.
Aphakia is the absence of the natural crystalline lens.
The aphakic state is usually due to surgery to remove a cataractous lens.
The aphakic state post-surgically is rare nowadays because of the ubiquity of intraocular lenses.
Aphakia can be post-traumatic or congenital in nature, but is rare.
Aphakic IOL refers to a lens implanted secondarily in an eye already aphakic from previous surgery or trauma.
Pseudophakia is the substitution of the natural crystalline lens with an IOL.
A posterior chamber IOL (PCIOL) is the most common type of implanted lens after cataract surgery, as this is the natural and optimum position for a lens.
The Anterior chamber IOL is less-common type of intraocular lens, used if a PCIOL is not an option for a patient or if the situation requires a phakic IOL (PIOL).
Pseudophakic IOLs are lenses implanted during cataract surgery, immediately after removal of the patient’s crystalline lens.
Monofocal IOLs are standard lenses used in cataract surgery.
The disadvantages of these conventional IOLs is that they can only be focused for one particular distance – either optical infinity or a fixed finite distance.
Patients who undergo a standard IOL implantation are unable to accommodate-change focus from near to far, far to near, and to distances in between.
For most cataract surgeries performed on elderly people who are already completely presbyopic, this is not a problem.
For patients that are not yet presbyopic undergoing refractive lens exchange for the sake of correcting refractive errors, it can be a problem.
Monovision, in which one eye is made emmetropic and the other myopic, can partially compensate for the loss of accommodation and enable clear vision at multiple distances.
Multifocal IOLs attempt to provide simultaneous viewing of distance vision and near vision.
Trifocal IOLs can provide intermediate vision in addition.
Concentric ring multifocal lenses are prone to glare and mildly compromised focus at all ranges of vision.
People who have a multifocal IOL after their cataract is removed may be less likely to need additional glasses compared with people who have standard monofocal lenses.
The most common adverse visual effects from multifocal IOLs include glare, halos and a loss of contrast sensitivity in low-light conditions.
An adjustable IOL allows its prescription power can be adjusted after surgery once all healing is complete, while all other IOLs require surgeons to use pre-surgery measurements to determine a patient’s post-surgery lens power.
Pre-surgery measurements are taken while a patient still has cataracts, and they do not account for minuscule shifts that occur during healing.
The adjustable IOL allows surgeons to implant it and then, once healing is complete, use an ultraviolet light delivery device to fine tune it.
After the eye has healed, usually 2 to 4 weeks after IOL implantation, refraction adjustment is done.
Customization of the IOL’s refractive power is done by exposing either the lens to a metered dose of UV light, with the help of a contact lens on the cornea.
Meridional exposure can be done to correct for astigmatism.
Some newer lens designs attempt to allow the eye to regain some ability to change focus from distance to near accommodation.
Many accommodating IOLs used today only achieve a very limited improvements in near vision which reduced over time.
Posterior capsule opacification (PCO), is a common side-effect of many cataract surgeries and is easily treatable with a one-time laser capsulotomy procedure.
Accommodating IOLs interact with ciliary muscles and zonules, by hinges at both ends to latch onto and move forward and backward inside the eye using the same nerves and musculatur as normal accommodation.
An accommodating lens is implanted in the eye’s lens capsule, where the contractions of the ciliary body which would focus the eye with the natural lens are used to focus the implant.
A toric IOL is a type of toric lens used to correct preexisting corneal astigmatism at the time of cataract surgery.
Astigmatism can also be treated with limbal relaxing incisions or an excimer laser procedure.
About 40% of Americans have significant astigmatism and thus may be candidates for a toric IOL.
Toric IOLs have different powers in different meridians of the lens, and they must be positioned on the correct meridian to reverse the preexisting astigmatism.
If the toric IOL is not on the correct meridian, it may need to be repositioned in a second procedure.
Multifocal toric IOLs provide correction of preexisting astigmatism, but also with multiple-focused vision at far and reading distance.
Extended depthintraocular lens technology is used for treating presbyopia.
These lenses are intended to have little effect on distance vision, and improve middle distance and near vision.
Phakic IOLs (PIOLs) are intraocular lenses which are placed in an eye that still contains a natural human crystalline lens.
Phakic IOLs can be either spheric or toric. Toric PIOLs have to be aligned with the meridian of astigmatism; toric IOL misalignment or rotation can lead to residual or even greater astigmatism postoperatively.
PIOLs can be divided into three categories:
Angle-supported PIOLs, placed in the anterior chamber.
They have a negative impact on the corneal endothelial lining, which is vital for maintaining a healthy clear cornea.
Iris-fixated PIOLs, attached by claws to the mid-peripheral iris.
Iris-fixated PIOLs believed to have a lesser effect on corneal endothelium, but a tendency to cause endothelial cell reduction.
Blue light filtering IOLs filter the UV and high-energy blue light present in natural and artificial light.
Posterior capsule opacification (PCO), often is the most common complication of cataract surgery.
Posterior chamber intraocular lenses may form PCOs a few months after implantation.
PCOs are easily treatable, and only require a one-time capsulotomy procedure (using a Nd:YAG laser) to clarify.
The materials that have been used to manufacture intraocular lens implants include poly(methyl methacrylate) (PMMA), silicone, hydrophobic acrylate, hydrophilic acrylate and collamer.
The use of silicone and acrylic polymers, are soft foldable inert materials, allowing the lens to be folded and inserted into the eye through a smaller incision.
The appropriate refractive power of the IOL is selected to provide the desired refractive outcome.
Pre-operative measurements, including corneal curvature, axial length are used to estimate the required power of the IOL.
