 2378
2378
Lies between adjacent vertebrae in the vertebral column.
Each disc forms a fibrocartilaginous joint, to allow slight movement of the vertebrae, and acts as a ligament to hold the vertebrae together.
Role as shock absorbers.
Discs consist of an outer fibrous ring, the anulus fibrosus disci intervertebralis, which surrounds an inner gel-like center, the nucleus pulposus.
The anulus fibrosus consists of several layers of fibrocartilage made up of both type I and type II collagen.
Type I is concentrated towards the edge of the ring where it provides greater strength.The nucleus pulposus and this helps to distribute pressure evenly across the disc, preventing the development of stress concentrations which could cause damage to the underlying vertebrae or to their endplates.
The nucleus pulposus contains loose fibers suspended in a mucoprotein gel.
The nucleus of the disc acts as a shock absorber, keeps the two vertebrae separated, and is the remnant of the notochord.
There is one disc between each pair of vertebrae, except for the first cervical segment, the atlas.
The atlas is a ring around the roughly cone-shaped extension of the axis, the second cervical segment.
The axis acts as a post around which the atlas can rotate, allowing the neck to swivel.
There are 23 discs in the human spine: 6 in the cervical region, 12 in the thoracic region, and 5 in the lumbar region.
Vertebral discs have some vascular supply to the cartilage endplates and the annulus fibrosus, that quickly deteriorate leaving almost no direct blood supply in healthy adults..
The intervertebral disc functions to separate the vertebrae from each other and provides the surface for the shock-absorbing gel of the nucleus pulposus.
The nucleus pulposus of the disc functions to distribute hydraulic pressure in all directions within each intervertebral disc under compressive loads.
Events closing intravertebral disc include a genetic basis, and previous spinal trauma.
The nucleus pulposus consists of large vacuolated notochord cells, small chondrocyte-like cells, collagen fibrils, and aggrecan, a proteoglycan that aggregates by binding to hyaluronan.
The nucleus pulposus contains collagen and elastin fibers imbedded within a hydrated proteoglycan gel.
Attached to each aggrecan molecule are glycosaminoglycan (GAG) chains of chondroitin sulfate and keratan sulfate.
Aggrecan is highly negatively charged, allowing the nucleus pulposus to swell by imbibing water, and the amount of glycosaminoglycans and water decreases with age and degeneration.
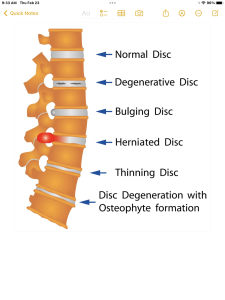
A spinal disc herniation can occur when the gel-like material of the nucleus pulposus is forced against a weakness in the surrounding anulus fibrosus, putting pressure on the nearby nerve giving symptoms.
Another kind of herniation, of the nucleus pulposus, can also happen as a result of the formation of Schmorl’s nodes on the intervertebral disc, referred to as vertical disc herniation.
Before age 40 approximately 25% of people show evidence of disc degeneration at one or more levels, while beyond age 40, more than 60% of people show evidence of disc degeneration at one or more levels on magnetic resonance imaging (MRI).
With aging and disc degeneration the nucleus pulposus begins to dehydrate and the concentration of proteoglycans in the matrix decreases, thus limiting the ability of the disc to absorb shock.
Shrinking of disc size is partially responsible for the decrease in height as humans age.
The anulus fibrosus also becomes weaker with age and has an increased risk of tearing.
With age the cartilage endplates thin, fissures begin to form, and there is sclerosis of the subchondral bone.
As the fissures are formed in the anulus fibrosis due to osteo-arthritic bones or degeneration in general, the inner nucleus pulposus can seep out and put pressure on vertebral nerves.
Discogenic pain is attributable to pain signals arising from nerves in the outer layers of the disc (annulus fibrosus).
Outer tears in the annulus fibrosus stimulate nociceptors and inflammatory mediators.
LBP pain may also become from nucleus pulposus and vertebral endplates that might irritate the annulus of the intervertebral disc.
A herniated disc can cause mild to severe pain.
A herniated disc treatment can range from surgery to physical therapy.
Degeneration of the vertebral column includes diffuse idiopathic skeletal hyperostosis which is the calcification or ossification of the ligaments surrounding the vertebrae.
Degeneration of the vertebral column causes stiffness and sometimes even curvature in the lumbar and thoraco-lumbar spinal region.
Patients with scoliosis commonly have calcium deposits in the cartilage endplate and sometimes in the disc itself.
Disc degeneration is associated with annular tears and dehydration of the nucleus pulposus that can lead to decreased disc height, impaired mechanical function, rupture, and compression of the spinal nerve roots.
Nerve and vascular in growth into the disc and exposure of these nerves to inflammatory mediators is associated with axial low back pain.
In addition to scoliosis, the fused vertebrae can also experience other abnormalities such as kyphosis which shows in old age, or lordosis which is often present in pregnancy and obesity.
The intervertebral disc space is typically defined on an X-ray photograph as the space between adjacent vertebrae, and corresponds to the size of the intervertebral disc.
The intervertebral disc space size can be altered in pathological conditions such as discitis
Loss of disk height narrows foramina, through which nerve roots exit the spinal column, and leads to circumferential bulging of the annulus.
