 Cardiac implantable electronic devices, include: pacemakers, implantable cardioverter defibrillator (ICD), biventricular pacemakers, and cardiac loop recorders.
Cardiac implantable electronic devices, include: pacemakers, implantable cardioverter defibrillator (ICD), biventricular pacemakers, and cardiac loop recorders.
Cardiac implantable electronic devices (CIEDs) constitute improvement in the management of heart rhythm disorders.
Increasingly common management process for chronic heart disease.
Estimate is that one and a half million patients receive cardiac implantable electronics devices worldwide every year.
They are designed to help control or monitor irregular heartbeats in people with certain heart rhythm disorders and heart failure.
These devices continuously collects information about the heart’s rhythm. Devices include bradycardia pacemakers, biventricular pacemakers implantable cardioverter-defibrillators (ICDs).
An artificial pacemaker works by supporting the heart’s natural rhythm.
Indications for bradycardia pacemakers include sick sinus syndrome and type II degree block, high-grade, and complete heart block.
An artificial implantable cardioverter defibrillator (AICD) can recognize a dangerous heart rhythm and send messages to the heart to try and slow the rhythm and return it to normal.
If this doesn’t work, the AICD can send an electric shock to jolt the heart out of its ventricular fibrillation.
Problems with the electrical circuitry of the heart can include blocked signals or signals taking an abnormal path through the heart.
An artificial pacemaker is an implantable device that mimics the actions of the nodes and conducting system, and helps to regulate the heart rate.
An implantable cardioverter defibrillator (AICD) can recognize a dangerous heart rhythm and send messages to the heart to try and slow the rhythm and return it to normal.
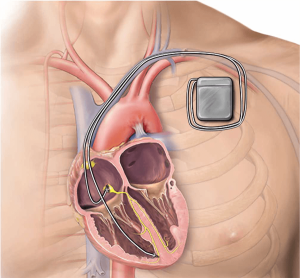
An artificial cardiac pacemaker is a small battery-operated computer, called a pulse generator, which is connected to the heart by one or more leads.
These leads are made of a coiled metal conductor, that are insulated with plastic and fixed to the inner wall of the heart.
The pulse generator sends an electrical down the lead to an electric conductor attached to the heart, causing the heart chamber to contract.
The artificial pacemaker monitors the heart and increases the heart’s rate as needed.
The pulse generator may have sensors to detect physical activity or changes in breathing.
The two major types of artificial cardiac pacemakers include:
single chamber – only one chamber is regulated, usually the ventricles.
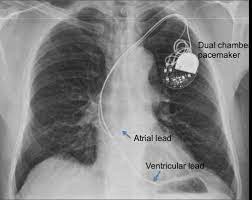
dual chamber – two leads are used.
Information from the atria regulates the contractions of the ventricles.
The traditional model is placed under the skin and connects to the heart via electronic leads.
A smaller, leadless pacemaker is placed inside the heart and does not require transvenous leads.
Pacemakers are used to manage bradycardia, a condition that causes the heart to beat too slowly—less than 60 beats per minute.
The pacemaker produces electrical pulses that keep the heart beating at a normal rate.
A biventricular pacemaker works like a conventional pacemaker but uses a third wire to send electrical impulses to the heart to resynchronize the contractions of the heart’s left lower chambers, or ventricles.
Also called a cardiac resynchronization device, a biventricular pacemaker is implanted when medications don’t relieve symptoms of heart failure, and when the left chamber does not beat in a coordinated manner.
The typical hospital stay for artificial cardiac pacemaker implantation is between one to two days.
The procedure is usually done under local anaesthesia.
The pulse generator, is generally implanted under the skin just below the collarbone on either the right or left side.
The leads are inserted using x-ray control, via a vein found in this area, and positioned in the appropriate right-sided heart chamber.
The leads are tested before the pulse generator is attached and the incision is closed.
Working, driving a car and light exercise can resume after one to two weeks recovery.
Artificial implantable cardioverter defibrillator (AICD)
AICD complex device that can recognize a dangerous heart rhythm and send messages to regulate the heart.
If this doesn’t work, the AICD can send an electric shock to jolt the heart out of its fibrillation.
People with advanced heart disease, heart failure and certain genetic arrhythmias are often at risk of life-threatening, fast, irregular heartbeats called ventricular arrhythmias, may need an ICD, which delivers an electric shock to restore a normal heart rhythm.
An ICD is often recommended for people with ventricular arrhythmias that have not responded to other treatment, such as catheter ablation or medical therapy.
Biventricular defibrillators are for people who would benefit from resynchronization yet also require the protection of a defibrillator.
Biventricular defibrillators work to maintain a steady heartbeat and either speed up or slow down a heart that is beating too slow or too fast.
Implantable Cardiac Loop Recorders
A wireless cardiac monitor called a loop recorder continuously records information about your heart’s rhythm for up to three years.
The implantable cardiac loop recorder is inserted beneath the skin of the upper chest to record information about the heart’s electrical activity, much like an electrocardiogram
The implantable cardiac loop recorder is is used to diagnose or identify the source of an arrhythmia.
Cardiac implantable electronic devices, include: pacemakers, implantable cardioverter defibrillator (ICD), biventricular pacemakers, and cardiac loop recorders.
They are designed to help control or monitor irregular heartbeats in people with certain heart rhythm disorders and heart failure.
These devices continuously collects information about the heart’s rhythm.
An artificial pacemaker works by supporting the heart’s natural rhythm.
An artificial implantable cardioverter defibrillator (AICD) can recognize a dangerous heart rhythm and send messages to the heart to try and slow the rhythm and return it to normal.
If this doesn’t work, the AICD can send an electric shock to jolt the heart out of its ventricular fibrillation.
Problems with the electrical circuitry of the heart can include blocked signals or signals taking an abnormal path through the heart.
An artificial pacemaker is an implantable device that mimics the actions of the nodes and conducting system, and helps to regulate the heart rate.
An implantable cardioverter defibrillator (AICD) can recognize a dangerous heart rhythm and send messages to the heart to try and slow the rhythm and return it to normal.
An artificial cardiac pacemaker is a small battery-operated computer, called a pulse generator, which is connected to the heart by one or more leads.
These leads are made of a coiled metal conductor, that are insulated with plastic and fixed to the inner wall of the heart.
The pulse generator sends an electrical down the lead to an electric conductor attached to the heart, causing the heart chamber to contract.
The artificial pacemaker monitors the heart and increases the heart’s rate as needed.
The pulse generator may have sensors to detect physical activity or changes in breathing.
The two major types of artificial cardiac pacemakers include:
single chamber – only one chamber is regulated, usually the ventricles.
dual chamber – two leads are used.
Information from the atria regulates the contractions of the ventricles.
The traditional model is placed under the skin and connects to the heart via electronic leads.
A smaller, leadless pacemaker is placed inside the heart and does not require transvenous leads.
Pacemakers are used to manage bradycardia, a condition that causes the heart to beat too slowly—less than 60 beats per minute.
The pacemaker produces electrical pulses that keep the heart beating at a normal rate.
A biventricular pacemaker works like a conventional pacemaker but uses a third wire to send electrical impulses to the heart to resynchronize the contractions of the heart’s left lower chambers, or ventricles.
Also called a cardiac resynchronization device, a biventricular pacemaker is implanted when medications don’t relieve symptoms of heart failure, and when the left chamber does not beat in a coordinated manner.
The typical hospital stay for artificial cardiac pacemaker implantation is between one to two days.
The procedure is usually done under local anaesthesia.
The pulse generator, is generally implanted under the skin just below the collarbone on either the right or left side.
The leads are inserted using x-ray control, via a vein found in this area, and positioned in the appropriate right-sided heart chamber.
The leads are tested before the pulse generator is attached and the incision is closed.
Working, driving a car and light exercise can resume after one to two weeks recovery.
Artificial implantable cardioverter defibrillator (AICD)
AICD complex device that can recognize a dangerous heart rhythm and send messages to regulate the heart.
If this doesn’t work, the AICD can send an electric shock to jolt the heart out of its fibrillation.
People with advanced heart disease, heart failure and certain genetic arrhythmias are often at risk of life-threatening, fast, irregular heartbeats called ventricular arrhythmias, may need an ICD, which delivers an electric shock to restore a normal heart rhythm.
An ICD is often recommended for people with ventricular arrhythmias that have not responded to other treatment, such as catheter ablation or medical therapy.
Biventricular defibrillators are for people who would benefit from resynchronization yet also require the protection of a defibrillator.
Biventricular defibrillators work to maintain a steady heartbeat and either speed up or slow down a heart that is beating too slow or too fast.
Implantable Cardiac Loop Recorders
A wireless cardiac monitor called a loop recorder continuously records information about your heart’s rhythm for up to three years.
The implantable cardiac loop recorder is inserted beneath the skin of the upper chest to record information about the heart’s electrical activity, much like an electrocardiogram
The implantable cardiac loop recorder is is used to diagnose or identify the source of an arrhythmia.
Pacemaker or cardioverter-defibrillator infection affects approximately 1.4 to 2.5% of such patients.
Infection is a recognized complication of such device implantation and there has been a marked increase in infections.
Patients with a cardiac implantable electronic device that present with any symptoms or sign of systemic infection should be evaluated for a device related infection.
Infection necessitates complete device removal and pathogen directed antimicrobial drug therapy.
Cardiac implantable electronic device infections can occur at the device pocket site, the leafs, and/or the endocardial surfaces.
Infections of CIEDs can result in increased mortality ranging between 12 and 22%.
Increased risk of infections associated with age, coexisting diabetes, device revision, heart failure, corticosteroid use and use of anticoagulant at the time of implantation with high rates of pocket hematomas.
Managing infections are costly with an estimated cumulative infection management cost as high as $279,000 for initial implants at 362,000 for replacements.
Device infections are associated with significant in-hospital and long-term mortality.
Fever within 24 hours preceding the device implantation, utilization of a temporary transient space maker, need to remove pocket hematoma, wound dehiscence, and failure to use at a biotic prophylaxis all increase risk of infection.
Increase in device lead number and longer implant times may also be associated with increased risk of infections, and physician procedure volume experience is inversely correlated with risk of infection.
Device variations may be associated with increased bacterial seeding.
CIED infection has worse outcomes for staphylococcal infections.
Most CIED infections are caused by Gram positive organisms, particularly staphylococcal bacteria.
Diagnosis relies on blood culture and echocardiography.
Transesophageal echocardiography has a higher sensitive for detecting lead and valvular vegetations compared with transthoracic echocardiography.
PET/CT can help in diagnosing cardiac implantable electronic device infections.
Gram negative bacteria represent about 10% of device infections.
Gram negative bacteria CIED infections are usually present with a localized pocket infection.
Untreated gram-negative CIED pocket infections may progress to blood systemic infection by hematogenous spread, but is rare.
After explantation, oral Antibiotic drug management is a reasonable choice for pocket infections due to Gram negative bacteria.
Adjunctive use of an antibacterial envelope results in a 40% lower incidence of major CIED infection and standard of care infection-prevention strategies alone (WRAP-IT investigators).
Treatment of infected pacemaker or cardioverter-defibrillators includes antibiotics with or without device removal and insertion of a temporary electrode connected to an external pacemaker unit to support heart rate.
