Hypersensitivity, also called hypersensitivity reaction or intolerance is an abnormal physiological condition in which there is an undesirable and adverse immune response to antigen.
It is an abnormality in the immune system that causes immune diseases including allergies and autoimmunity.
It is caused by many types of particles and substances from the external environment or from within the body that are recognized by the immune cells as antigens.
The immune reactions are an over-reaction of the immune system and they are often damaging and uncomfortable.
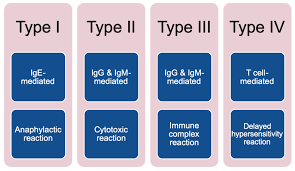
Gell and Coombs classification :four types of hypersensitivity, namely, type I, which as an IgE mediated immediate reaction; type II, an antibody-mediated reaction mainly involving IgG or IgM; type III, an immune complex-mediated reaction involving IgG, complement system and phagocytes; type IV, a cytotoxic, cell-mediated, delayed hypersensitivity reaction involving T cells.
The first three types are considered immediate hypersensitivity reactions because they occur within 24 hours.
The fourth type is a delayed hypersensitivity reaction because it usually occurs more than 12 hours after exposure to the allergen.
The fourth type has a maximal reaction time between 48 and 72 hours.
Hypersensitivity is a common occurrence.
About 15% of people have at least one hypersensitivity type reaction during their lives, and has increased since the latter half of the 20th century.
Type I HSR:
Type I hypersensitivity occurs as a result of exposure to an antigen.
The antigens are proteins with a molecular weight ranging from 10 to 40 kDa.
The response to the antigen occurs in two stages: the sensitization and the effect stage.
In the sensitization stage, the host experiences an asymptomatic contact with the antigen.
In the effect period, the pre-sensitized host is re-introduced to the antigen, which then leads to a type I anaphylactic or atopic immune response.
Types of antigens involved
Food: nuts, eggs, soy, wheat, shellfish, etc.
Animal source: bees, wasp, cats, insects, rats.
Environmental factors: dust mites, latex, pollen, mold, and flowers smell.
Atopic diseases: allergic asthma, allergic rhinitis, conjunctivitis, dermatitis.
Medication-induced reactions: antibiotics
Fast response which occurs in minutes, rather than multiple hours or days.
Free antigens cross link the IgE on mast cells and basophils which causes a release of vasoactive biomolecules.
Testing can be done via skin test for specific IgE.
Associated with
Atopy
Anaphylaxis
Asthma
Churg–Strauss Syndrome
Type II HR
Antibody-dependent
Antibody IgM
Antibody IgG
Complement
Membrane attack complex (MAC):
Antibody (IgM or IgG) binds to antigen on a target cell, which is actually a host cell that is perceived by the immune system as foreign, leading to cellular destruction via the MAC.
Testing includes both the direct and indirect Coombs test.
Autoimmune hemolytic anemia
Rheumatic heart disease
Thrombocytopenia
Erythroblastosis fetalis
Goodpasture’s syndrome
Graves’ disease
Myasthenia
Pemphigus vulgaris
III HR
Type II hypersensitivity
Type II hypersensitivity reaction refers to an antibody-mediated immune reaction in which antibodies (IgG or IgM) are directed against cellular or extracellular matrix antigens with the resultant cellular destruction, functional loss, or damage to tissues.
The antigens may be glycoproteins on the cell membrane of erythrocytes that are key molecules that determine blood types.
Depending on the chemical nature of the antigens, blood types have different levels of hypersensitivity; for instance, A and B are more antigenic than other antigens.
Type II hypersensitivity damage can be accomplished via three different mechanisms:
Antibody binding to cell surface receptors and altering its activity
Activation of the complement pathway.
Antibody-dependent cellular cytotoxicity.
The pathophysiology of type II hypersensitivity reactions can be broadly classified into three types:
Cell depletion or destruction without inflammation
Inflammation mediated by complement or Fc receptor
Cellular dysfunction by antibodies
The process involves a series of immune-mediated events:
Immune complex
Antibody IgG
Complement
Neutrophils
Antibody (IgG) binds to soluble antigen, forming a circulating immune complex.
This is often deposited in the vessel walls of the joints and kidney, initiating a local inflammatory reaction.
Serum sickness
Rheumatoid arthritis
Arthus reaction
Post streptococcal glomerulonephritis
Membranous nephropathy
Reactive arthritis
Lupus nephritis
Systemic lupus erythematosus
Extrinsic allergic alveolitis (hypersensitivity pneumonitis)
Type III hypersensitivity reactions:
serum sickness, post-streptococcal glomerulonephritis, systemic lupus, and rheumatoid arthritis.
The principal feature that separates type III reactions from other hypersensitivity reactions is that in type III reaction, the antigen-antibody complexes are pre-formed in the circulation before their deposition in tissues.
In type III hypersensitivity reaction, an abnormal immune response is mediated by the formation of antigen-antibody aggregates called immune complexes.
They can precipitate in various tissues such as skin, joints, vessels, or glomeruli, and trigger the classical complement pathway.
Complement activation leads to the recruitment of inflammatory cells (monocytes and neutrophils) that release lysosomal enzymes and free radicals at the site of immune complexes, causing tissue damage.
In type III hypersensitivity reaction, an abnormal immune response is mediated by the formation of antigen-antibody aggregates called immune complexes.
They can precipitate in various tissues such as skin, joints, vessels, or glomeruli, and trigger the classical complement pathway.
Complement activation leads to the recruitment of inflammatory cells (monocytes and neutrophils) that release lysosomal enzymes and free radicals at the site of immune complexes, causing tissue damage.
Type IV hypersensitivity
Delayed, cell-mediated immune memory response,
Antibody-independent
Cytotoxic
Cells
T-cells
CTL’s and T helper cells,specifically Th1 and Th17 cells,are activated by an antigen presenting cell.
When the antigen is presented again in the future, the memory Th1 cells will activate macrophages and cause an inflammatory response.
This ultimately can lead to tissue damage.
Contact dermatitis, including Urushiol-induced contact dermatitis (poison ivy rash).
Mantoux test
Chronic transplant rejection
Multiple sclerosis
Celiac disease
Hashimoto’s thyroiditis
Granuloma annulare
Type IV hypersensitivity reactions are, to some extent, normal physiological events that help fight infections, and dysfunction in this system can predispose to multiple opportunistic infections.
Adverse events can also occur due to these reactions when an undesirable interaction between the immune system and an allergen happens.
A type IV hypersensitivity reaction is mediated by T cells that provoke an inflammatory reaction against exogenous or endogenous antigens.
In certain situations, other cells, such as monocytes, eosinophils, and neutrophils, can be involved in type IV hypersensitivity
After antigen exposure, an initial local immune and inflammatory response occurs that attracts leukocytes.
The antigen engulfed by the macrophages and monocytes is presented to T cells, which then becomes sensitized and activated.
These cells then release cytokines and chemokines, which can cause tissue damage and may result in illnesses.
Examples of illnesses resulting from type IV hypersensitivity reactions include contact dermatitis and drug hypersensitivity.
Type IV reactions are further subdivided into type IVa, IVb, IVc, and IVd based on the type of T cell (Th1, Th17, and CTLs) involved and the cytokines/chemokines produced.
Delayed hypersensitivity plays a crucial role in the ability to fight various intracellular pathogens such as mycobacteria and fungi, and in tumor immunity and transplant rejection.
In patients with acquired immunodeficiency syndrome (AIDS) have a progressive decline in the number of CD4 cells and also have a defective type four hypersensitivity reaction.
Treatment of immediate hypersensitivity reactions includes the management of anaphylaxis with intramuscular adrenaline, oxygen, intravenous (IV) antihistamine, support blood pressure with IV fluids, avoid latex gloves and equipment in patients who are allergic, and surgical procedures such as tracheotomy if there is severe laryngeal edema.
Allergic bronchial asthma can be treated with any of the following: inhaled short- and long-acting bronchodilator anticholinergics along with inhaled corticosteroids, leukotriene antagonists, use of disodium cromoglycate, and environmental control.
Experimentally, a low dose of methotrexate or cyclosporine and omalizumab, a monoclonal anti-IgE antibody, has been used.
Treatment of autoimmune disorders include one or a combination of NSAIDs and hydroxychloroquine, azathioprine, methotrexate, mycophenolate, cyclophosphamide, low dose IL-2, intravenous immunoglobulins, and belimumab.
Omalizumab is a monoclonal antibody that interacts with the binding site of the high-affinity IgE receptor on mast cells.
It is an engineered, humanized recombinant immunoglobulin.
Moderate to severe allergic bronchial asthma can improve with omalizumab.
Treatment of type 4 HR involves the treatment of the eliciting cause.
The most common drugs to treat tuberculosis include isoniazid, rifampin, ethambutol, pyrazinamide, amikacin, kanamycin, or capreomycin.
The most common drugs to treat leprosy include rifampicin and clofazimine in combination with dapsone for multibacillary leprosy.
A single dose of antimicrobial combination to cure single lesion paucibacillary leprosy comprises ofloxacin, rifampicin, and minocycline.
Praziquantel can be useful for treating infections caused by all Schistosoma species.
Hydroxychloroquine and chloroquine can use in the therapy of sarcoidosis involving the skin, lungs, and the nervous system.
The use of anti-TNF monoclonal antibodies such as adalimumab and certolizumab have been approved for Crohn disease.
