Disease is the predominant cause of disability and death in the U.S. and accounts for 40% of all postnatal deaths, about 750,000, annually.
The heart pumps blood that delivers life-sustaining oxygen and nutrients to 300 trillion cells.
Each day the average heart beats 100,000 times and pumps about 2,000 gallons of blood.
In a 70-year lifetime, an average human heart beats more than 2.5 billion times.
Weighs on the average of 250 -300 gm in females and 300-350 gm in males.
Thickness of the right ventricle is 0.3-0.5 cm and that of the left ventricle is 1.3-1.5 cm.
An increase in the heart size or weight is ref2242ed to associated cardiomegaly.
Increased ventricular weight indicates the presence of hypertrophy.
Enlarged chamber size implies cardiac dilation.
The cardiac muscle, made of cardiac myocytes, specialized muscle cells arranged in a circumferential and spiral orientation around the left ventricle.
Is a functional syncytium, propagating electrical impulses between communicatingncells so that the various components of the heart act as a single contractile apparatus.
Cardiomyocytes are the contractile cells that make up heart muscle, and form the syncytium of unified contractile function.
The hearts propagates electrical impulses between communicating cells so it can function as a syncytium and can act as a single contractile apparatus.
Cardiomyocytes are made up of specialized components to include sarcomeres, extensive mitochondria, and junctional complexes, and are responsible for maintaining biochemical stores to meet energy demands placed on the cells.
Cardiomyocytes are very differentiated, and as a result have very limited regenerative potential.
Cardiomyocyte function depends on a critical balance between protein synthesis, protein folding, and protein turnover.
Although cardiomyocytes can be renewable, approximately one gram of myocardial mass, corresponding to 64 million cells, is lost per year in the human heart.
Heat -shock proteins (HSP) family of chaperones are expressed in the heart.
The most abundant chaperone in the heart is known as HSPB5, also known as Alpha Beta-crystalline (CryAB).
CryAB is associated with cytoskeletal and contractile apparatus proteins in cardiac muscle cells.
CryAB interacts with desmin, a critical protein in cardiomyocytes preventing its mis-folding and aggregation.
The sinoatrial pacemaker, the sinoatrial node, the atrioventricular node, the bundle of HIS and the right and let bundle branches are specialized excitatory and conducting myocytes that control the rate and rhythm of the heart.
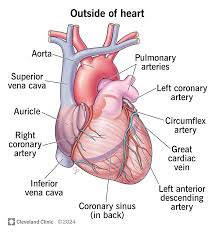
Blood supply to the heart begin at the aorta, immediately distal to the aortic valve in the sinuses of Valsalva.
The coronary arteries are 2-4 mm diameter vessels that are 5-10 cm long that run along the external surface of the heart.
The epicardial coronary arteries penetrate into the myocardium as intramural arteries that yield arterioles and capillaries in which nearly one vessel is adjacent to each cardiac muscle cell.
There are four cardiac valves that maintain unidirectional blood flow.
With age the amount of fat in the epicardium increases, particularly over the anterior surface of the right ventricle and in the atrium septum.
The left ventricle cavity decreases in size with age, particularly in the base to apex dimension, and this is increased by the presence of hypertension.
With aging heart valves develop increasing calcification of the mitral annulus and aortic valve, increasing fibrous thickening and mitral leaflets tend to buckle toward the left atrium during ventricle systole simulating prolapse.
Myocyte is a terminally differentiated cell without the ability to divide.
Increase in myocte number is not possible but increase in mechanical load causes increased sucellular components and increase in cell size, known as hypertrophy.
Increased mechancial work increases the rate of protein synthesis and myocyte protein including the number of sarcomeres and mitochondria and mass of myocytes so that the size of the heart increases.
Action potential in the heart increases the level of intracellular calcium by two mechanisms, firstly, extracellular calcium enters the cell through L-type calcium channels increasing intracellular calcium concentration, which leads to type 2 ryanodine receptor opening and release of calcium from the sarcoplasmic reticulum.
Secondly, reversal of these changes occurs during cardiac relaxation i.e. diastole, with the removal of calcium to the extracellular space with the extrusion of calcium through the sodium-calcium exchanger and re-uptake of calcium into the sarcoplasmic reticulum through ryanodine receptor 2 closing and the through activation of isoform 2a of sarcoendoplasmic reticulum calcium ATPase.
Cardiac action potential consists of two cycles, a rest phase, and an active phase.
These two phases are commonly understood as systole and diastole.
The rest phase is considered polarized.
The resting potential during this phase of the beat separates the ions such as sodium, potassium, and calcium.
The myocardiocyte’s membrane allows sodium ions to slowly enter the cell until the threshold is reached for depolarization.
Calcium ions follow and extend the depolarization even further.
Once calcium stops moving inward, potassium ions move out slowly to produce repolarization.
The very slow repolarization of the cardiac muscle cell membrane is responsible for the long refractory period.
