Abnormal sounds heard in various parts of the vascular system, but most commonly denotes noise heard over the heart.
There has been a steady decline in both the teaching and proficiency of stethoscope use in auscultation skills among doctors.
Blood flow is laminar and silent but when blood flow becomes turbulent is creates sound.
Above a critical velocity blood flow becomes turbulent.
Blood flow speeds up when there is narrowing of a artery and heart valve takes place.
Major causes of cardiac murmurs is disease of heart valves.
Stenosis of a heart valve leads to acceleration and turbulence of blood flow.
Valve incompetence, regurgitation or insufficiency, leads to backward flow through a narrowed orifice that accelerated blood flow.
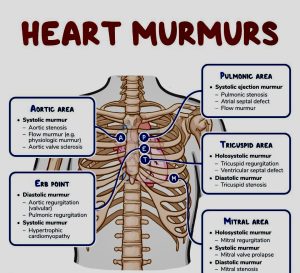
Best heard when the stethoscope is placed over the particular valve, such that disorders of the aortic and pulmonic valves are best heard at the base of the heart and murmurs due to the mitral valve are best heard at the apex.
Aortic and pulmonary valve stenosis murmurs are systolic, and insufficiency murmurs are diastolic in nature.
Mitral or tricuspid stenosis murmurs are diastolic and insufficiency murmurs are systolic.
Systolic heart murmurs are heart murmurs heard during systole and can be classified by when the murmur begins and ends, between S1 and S2.
Systoloic murmurs involve stenosis of the semilunar valves or regurgitation of the atrioventricular valves.
Mid-systolic ejection murmurs are due to blood flow through the semilunar valves and occur at the start of blood ejection, starting after S1 and ends with the cessation of the blood flow, which is before S2.
Midsystolic ejection murmur is a crescendo-decrescendo murmur and causes include outflow obstruction, increased flow through normal semilunar valves, dilation of aortic root or pulmonary trunk, or structural changes in the semilunar valves without obstruction.
Late systolic murmurs starts after S1 and, if left sided, extends up to S2, usually in a crescendo manner and causes include mitral valve prolapse, tricuspid valve prolapse and papillary muscle dysfunction.
Holosystolic murmurs start at S1 and extends up to S2.
They are usually due to regurgitation in cases such as mitral regurgitation, tricuspid regurgitation, or ventricular septal defect.
Regurgitation through the mitral valve is by far the most commonly heard murmur, producing a pansystolic/holosystolic murmur
Valvular aortic stenosis can produce a harsh, or even a musical murmur over the right second intercostal space which radiates into the neck over the two carotid arteries.
The most common cause of Aortic Stenosis is calcified valves due to aging and the second most common cause is congenital bicuspid aortic valvesu.
Bicuspid AS has little or no radiation of murmur.
The murmur in valvular Aortic stenosis decreases with standing and straining with Valsalva maneuver.
Supra aortic stenosis is loudest at a point slightly higher than in that of valvular AS and may radiate more to the right carotid artery.
Subvalvular aortic stenosis is usually due to hypertrophic cardiomyopathy (HCM), with murmur loudest over the left sternal border or the apex.
The murmur in HCM increases in intensity with a standing position as well as straining with Valsalva maneuver.
Pulmonic outflow obstruction is associated with a harsh murmur usually on left second intercostal space radiating to left neck and accompanied by palpable thrill, and a widely split S2.
Ventricular septal defect S2 is normal and it’s murmurs is almost always pansystolic where the murmur of pulmonary stenosis is diamond-shaped and ends clearly before S2.
Many innocent murmurs also arise from this location but S1 and S2 must split normally.
Dilation of aortic root or pulmonary artery produces a midsystolic ejection sound, with a short ejection systolic murmur and a relatively wide split S2.
Mid-systolic ejection Increased semilunar blood flow can occur in anemia, pregnancy, or hyperthyroidism.
Mid-systolic ejection aortic valve sclerosis due to degenerative thickening of the roots of the aortic cusps producing no obstruction and no hemodynamic effect, can be heard over right second intercostal space with a normal carotid pulse and normal S2.
Mid-systolic ejection innocent midsystolic murmurs are not accompanied by other abnormal findings.
Mitral valve prolapse is the most common cause of late systolic murmurs.
Mitral valve prolapse and is heard best over the apex of the heart, usually preceded by clicks.
If the prolapse becomes severe enough, mitral regurgitation may occur as well.
With mitral vave prolapse maneuvers that decrease left ventricular volume including standing, sitting, Valsalva maneuver, and amyl nitrate inhalation produce earlier onset of clicks, longer murmur duration, and decreased murmur intensity.
With mitral valve prolapse any maneuver that increases left ventricular volume including squatting, elevation of legs, hand grip, and phenylephrine can delay the onset of clicks, shorten murmur duration, and increase murmur intensity.
Holosystolic tricuspid insufficiency murmur intensifies upon inspiration, and is best heard over the fourth left sternal border.
The holosystolic murmur of tricuspid insufficiency intensity can be accentuated following inspiration, known as Carvallos sign due to increased regurgitant flow in right ventricular volume.
Tricuspid regurgitation is most often secondary to pulmonary hypertension, and less commonly due to bacterial endocarditis , Ebstein’s anomaly, carcinoid disease, or prior right ventricular infarction.
Mitral regurgitation associated with a holosystolic murmur without intensification upon inspiration.
The murmur in mitral regurgitation starts at the same time as S1 and can sometimes reach the sound of S2.
The murmur in mitral regurgitation is high pitched and best heard at the apex with patient in the lateral decubitus position.
Ventricular septal defect holosystolic murmur is not intensified by inspiration.
Ventricular systolic defect occurs in the ventricular wall, producing a shunt between the left and right ventricles, and since L ventricle has a higher pressure than the R ventricle, flow during systole occurs from the L to R ventricle, producing the holosystolic murmur.
Ventricular septal defect holosystolic murmur is best heard over the left third and fourth intercostal spaces and along the sternal border.
Ventricular septal defect holosystolic murmur is associated with normal pulmonary artery pressure and thus S2 is normal.
Ventricular septal defect holosystolic murmur can be distinguished from pulmonary stenosis, which has a wide splitting S2.
When the shunt becomes reversed in VSD , Eisenmenger syndrome, the murmur may be absent and S2 can become markedly accentuated and single.
Benign systolic heart murmur: benign paediatric heart murmur is ref2242ed to as Still’s murmur.
Diastolic heart murmur include pulmonic regurgitation (Graham Steell murmur) and aortic insufficiency (Austin Flint murmur) Carey Coombs murmur.
Childhood Innocent murmurs include a still murmur usually heard at the left side of the sternum in line with the nipple.
Pulmonic murmur is heard as blood flows into the pulmonary artery, best heard between the first two ribs on the left side of the sternum.
Venous hum heard as blood flows into the jugular veins of the neck, heard above the clavicle.
Characteristics of innocent murmurs in children include children of ages 3-7 years, the intensity of the murmur changes with the child’s position or breathing, and they are usually heard in one spot on the chest or above the clavicles and do not radiate to other areas like the armpits, back, or higher in the neck.
