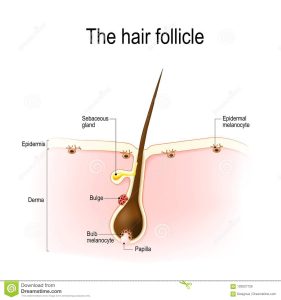
The hair follicle resides in the dermal layer of the skin and is made up of 20 different cell types, each with distinct functions.
The hair follicle regulates hair growth via a complex interaction between hormones, neuropeptides, and immune cells.
A hair follicle is a tube-like skin pore that encloses the shaft and root of the hair.
Most healthy adults have around 80,000–120,000 hairs on their scalps.
The hair follicle produces different types of hair on different parts of the body: terminal hair grow on the scalp and lanugo hairs are seen covering the bodies of fetuses in the uterus and in some newborn babies.
The process of hair growth occurs in distinct sequential stages: anagen is the active growth phase, catagen is the regression of the hair follicle phase, telogen is the resting stage, exogen is the active shedding of hair phase and kenogen is the phase between the empty hair follicle and the growth of new hair.
Humans have the longest growth phase of scalp hair compared to hair growth on other parts of the body.
Scalp hair defines appearance and also provides protection from UV sun rays and is an insulator against extremes of hot and cold temperatures.
Differences in the shape of the scalp hair follicle determine the observed ethnic differences in scalp hair appearance, length and texture.
Many diseases have abnormalities in hair appearance, texture or growth.
They may be early signs of local disease of the hair follicle or systemic illness.
Diseases of the hair follicle include alopecia, hirsutism and lupus erythematosus.
The position and distribution of hair follicles varies over the body.
The skin of the palms and soles does not have hair follicles whereas skin of the scalp, forearms, legs and genitalia has abundant hair follicles.
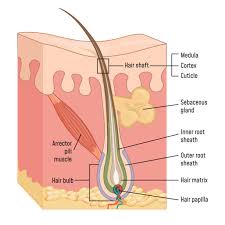
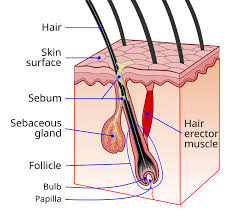
The triad of hair follicle, sebaceous gland and arrector pili muscle make up the pilosebaceous unit.
A hair follicle consists of :
The papilla is a large structure at the base of the hair follicle.
The papilla is made up mainly of connective tissue and a capillary loop.
Cell division in the papilla is either rare or non-existent.
Around the papilla is the hair matrix.
A root sheath composed of an external and internal root sheath.
The external root sheath appears empty with cuboid cells.
The internal root sheath is composed of three layers, Henle’s layer, Huxley’s layer, and an internal cuticle that is continuous with the outermost layer of the hair fiber.
The bulge is located in the outer root sheath at the insertion point of the arrector pili muscle.
The bulge houses several types of stem cells, which supply the entire hair follicle with new cells, and take part in healing the epidermis after a wound.
Other structures associated with the hair follicle include: the cup in which the follicle grows known as the infundibulum, the arrector pili muscles, the sebaceous glands, and the apocrine sweat glands.
Hair follicle receptors sense the position of the hair.
Attached to the follicle is a tiny bundle of muscle fiber called the arrector pili.
The arrector pili muscle is responsible for causing the follicle to become more perpendicular to the surface of the skin, and causing the follicle to protrude slightly above the surrounding skin causing piloerection.
This process results in goose bumps.
Atttached to the follicle is a sebaceous gland, which produces the oily or waxy substance sebum.
The higher the density of the hair, the more sebaceous glands that are found.
Ethnic differences exist in several different hair characteristics.
The differences in appearance and texture of hair are due to: the position of the hair bulb relative to the hair follicle, size and shape of the dermal papilla, and the curvature of the hair follicle.
The scalp hair follicle in Caucasians is elliptical in shape and, therefore, produces straight or wavy hair, whereas the scalp hair follicle of people of African descent is more curvy, resulting in the growth of tightly curled hair.
Ordinarily, hair follicle renewal is maintained by the stem cells associated with each follicle.
Aging of the hair follicle appears to be primed by a sustained cellular response to the DNA damage that accumulates in renewing stem cells during aging.
This damage response involves the proteolysis of type XVII collagen by neutrophil elastase in response to the DNA damage in the hair follicle stem cells.
Proteolysis of collagen leads to elimination of the damaged cells and then to terminal hair follicle miniaturization.
Hair grows in cycles of various phases:
anagen is the growth phase;
catagen is the involuting or regressing phase;
and telogen, the resting or quiescent phase.
Each phase has several morphologically and histologically distinguishable sub-phases.
Prior to the start of cycling is a phase of formation of the follicle.
There is also a shedding phase, or exogen, that is independent of anagen and telogen in which one or several hairs that might arise from a single follicle exits.
Normally up to 90% of the hair follicles are in anagen phase, while 10–14% are in telogen and 1–2% in catagen.
The cycle’s length varies on different parts of the body: eyebrows, the cycle is completed in around 4 months, while it takes the scalp 3–4 years to finish; this is the reason eyebrow hair have a much shorter length limit compared to hair on the head.
Growth cycles are controlled by a chemical signal like epidermal growth factor: DLX3 is a crucial regulator of hair follicle differentiation and cycling.
Anagen is the active growth phase of hair follicle.
During which the root of the hair is dividing rapidly, adding to the hair shaft.
During this phase the hair grows about 1 cm every 28 days.
Scalp hair stays in this active phase of growth for 2–7 years, and this period is genetically determined.
At the end of the anagen phase an unknown signal causes the follicle to go into the catagen phase.
The catagen phase is a short transition stage that occurs at the end of the anagen phase, and signals the end of the active growth of a hair.
This phase lasts for about 2–3 weeks while the hair converts to a club hair.
A club hair is formed during the catagen phase.
A club hair is formed when the part of the hair follicle in contact with the lower portion of the hair becomes attached to the hair shaft.
A bulb of keratin attaches to the bottom tip of the hair and keeps it in place while a new hair begins to grow below it.
A hair pulled out in this phase will have the bulb of keratin attached to it which appears as a small white ball on the end of the hair.
This process cuts the hair off from its blood supply and from the cells that produce new hair.
When a club hair is completely formed, about a 2-week process, the hair follicle enters the telogen phase.
The telogen phase is the resting phase of the hair follicle, about three months.
When the body is subjected to extreme stress, as much as 70 percent of hair can prematurely enter the telogen phase and begin to fall, causing a noticeable loss of hair.
This condition is called telogen effluvium.
The club hair is the final product of a hair follicle in the telogen stage, and is a dead, fully keratinized hair.
Fifty to one-hundred club hairs are shed daily from a normal scalp.
Scalp: The time these phases last varies from person to person.
Different hair color and follicle shape affects the timings of these phases.
Anagen phase, 2–8 years and occasionally much longer)
Catagen phase, 2–3 weeks
Telogen phase, around 3 months
Eyebrows:
Anagen phase, 4–7 months
Catagen phase, 3–4 weeks
Telogen phase, about 9 months
Many diseases in which abnormalities in hair appearance, texture or growth are early signs of local disease of the hair follicle or systemic illness.
Diseases of the hair follicle include alopecia or hair loss, hirsutism or excess hair growth, and lupus erythematosus.
Change in hair follicle microbiome result into scalp disease like; Seborrheic dermatitis of the scalp and dandruff, Folliculitis decalvans, Androgenetic alopecia, Scalp psoriasis and Alopecia areata.
Hair follicles form the basis of the two primary methods of hair transplantation in hair restoration, Follicular Unit Transplantation (FUT) and follicular unit extraction (FUE).
Naturally occurring groupings of one to four hairs, called follicular units, are extracted from the hair restoration patient and then surgically implanted in the balding area of the patient’s scalp, known as the recipient area.
These follicles are extracted from donor areas of the scalp typically resistant to the effects of the hormone DHT.
Miniaturization of the hair shaft from DHT that is the primary predictive indicator of androgenetic alopecia, commonly referred to as male pattern baldness or male hair loss.
When these DHT-resistant follicles are transplanted to the recipient area, they continue to grow hair in the normal hair cycle, thus providing the hair restoration patient with permanent, naturally-growing hair.
