 Vasculitis of unknown etiology that is common among elderly patients.
Vasculitis of unknown etiology that is common among elderly patients.
Affects large-sized and medium-sized vessels, most commonly the cranial arteries.
Improved imaging techniques- PET-CT scans, MRI and CT angiography has demonstrated an increased prevalence of extra-cranial involvement , termed large vessel GCA.
Prevalence of GCA estimated at 204 per hundred thousand population aged at least 50 years.
The presenting symptoms and findings of giant cell arteritis depend on the vessels involved and can include headache, scalp tenderness, vision loss, jaw claudication, as well as myalgias, andw symmetric stiffness of the shoulder and pelvic girdle.
Most common manifestation are cranial and ocular symptoms.
Can cause anterior ischemic optic neuropathy.
Predilection for aorta and its cranial branches.
Untreated approximately 50% of patients may go blind, with a smaller number having strokes, usually in the posterior circulation.
Most common systemic vasculitis affecting middle-aged and older people.
Minimal age of onset is 50 years, and the median age is in the seventh and eighth decade of life.
The presence of three or more of the following allow for diagnosis: age greater than 50 years at onset, new onset of headache, temporal artery abnormality with tenderness on palpation and decreased pulsation, elevated erythrocyte sedimentation rate of 50 mm per hour or higher, and an abnormal temporal artery biopsy.
Classic presentation includes headache, polymyalgia rheumatica, jaw claudication, and visual symptoms.
Jaw claudication, visual impairment, diplopia, arm claudication, and abdominal pain reflect blood vessel wall inflammation with luminal narrowing of arterial supply and ischemia.
40-60% of patients have symptoms of polymyalgia rheumatica.
Most patients have symptoms of vasculitis of the cranial arteries, similar involvement may be present in any large or medium sized artery, including the aorta and its branches.
It is the most common primary large vessel vasculitis affecting the aorta characterized by granulomatous inflammation affecting the muscle layer, although all layers of the aorta can be inflamed.
40% present with atypical manifestations such as ovarian or breast masses, SIADH, peripheral neuropathy, or mesentery ischemia (Levine SM, Hellman, DB).
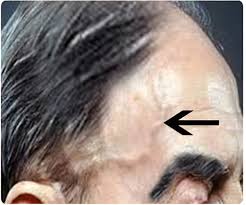
Skin manifestations include edema, urticaria, ulceration, purpura, and necrosis.
The temporal artery should be assesses for tenderness, extent of pulsation, or presence of bruits.
Mesenteric ischemia is uncommon.
Bowel infarction, aortic dissection or rupture may rarely occur.
Untreated disease may lead to a versatile loss of vision, primarily related to arteritic anterior ischemic optic neuropathy.
Death may be related to myocardial infarction, ischemic stroke, aortic aneurysm, aortic dissection, as well as complications of systemic therapy.
Erythrocyte sedimentation rate may be lower than 40 mm per hour in up to 20% of patients.
ESR higher than 50 mm/hr in more than 95% of patients, and more than 100 mm per hour in more than 40% (Gonzalez-Gay MA et al).
Patients with lower ESR associated with milder symptoms.
Up to 20% of patients with giant cell arteritis related vision loss do not have systemic symptoms, making the diagnosis difficult.
Some patients have symptoms of temporary vision loss, eye pain, or diplopia in the preceding weeks due to transit ischemia of the optic nerve head.
Frequently associated with elevated CRP, liver functions, especially alkaline phosphatase, hypoalbuminemia, anemia, reactive thrombocytosis, and increases immunoglobulin levels.
Because onset can be abrupt and irreversible vascular complications can occur the process is to be considered a medical emergency.
Ultrasound, PET/CT scans, MRI imaging can demonstrate vascular inflammation by vessel wall thickening and when used, tracer or contrast agent uptake.
Early diagnosis and treatment with glucocorticoids is the key to preventing complications.
Treatment consists of immunosuppression, typically with cotricosteroids.
Temporal artery biopsy is the most definitive test for diagnosis.
Consequence of unchecked disease is vision loss due to anterior ischemic optic neuropathy.
Arterial US is the first diagnostic test.
Color Doppler ultrasound of the temporal artery has a sensitivity and specificity of the halo sign- concentric, hypoechogenic, mural thickening caused by blood vessel edema in 69% and 82%, respectively.
PET/CT is most useful in patients with GCA with suspected involvement of the aorta and its major branches.
Glucocorticoids suppress vascular inflammation and prevent vascular complications.
Glucocorticoid therapy is associated with relapses in 34–62% of patients, and only 15–20% achieving long-term sustained remission with such therapy alone.
The usual management is glucocorticoid therapy.
Treatment is necessary to protect the unaffected eye as there an elevated risk of disease involvement.
The incidence of steroid related side effects, affecting up to 85% of GCA patients.
Large vessel GCA may be less responsive to corticosteroids.
GCA patients typically exceed a cumulative dose of 5000 mg prednisolone over several years.
The adverse event hazard ratio with corticosteroids rises by 3% for every 1000 mg increase.
Treatment with corticosteroids should not be withheld pending biopsy results in a patient with suspected disease since permanent visual impairment other than blindness occurs in 14% of patients and blindness occurs in up to 20% (Aiello).
Acute cases controlled with 40-60 mg of daily prednisone, and tapered over 9-12 months.
For patients with visual loss, aortitis or other widespread involvement require high dose corticosteroids.
Temporal artery biopsy 94-97% accurate for diagnosis.
Serial or bilateral temporal artery biopsies increase diagnostic yield by 3%.
Jaw claudication, scalp tenderness, new onset of headache and visual changes common findings in patients with giant cell arteritis.
Two-thirds of patients have headaches.
Headache pain is usually temporal, but may be frontal, occipital or generalized.
Headaches can wax and wane.
Tociluzumab approved for this arteritis.
Tocilizumab (TCZ), an IL-6 receptor inhibitor, is approved for use in GCA.
Tocilizumab is restricted to refractory and relapsing disease, those who have not received TCZ previously, and for a maximum of 1 year.
The phase III trial of TCZ (GiACTA), which formed the evidence base for its use, showed sustained glicocorticoid free remission in 56% and 53% of patients receiving weekly and fortnightly TCZ, respectively, both with a 26-week glucocorticoid taper.
This is compared with 14% and 18% in the 26-week and 52-week glucocorticoid taper placebo arms, respectively.
Upadacitinib a selective Janus kinase inhibitor (JAK) blocks the signaling of several cytokines, including IL-6 and interferon gamma.
Upadacitinib at a dose of 15 mg with a 26 glucocorticoid taper showed efficacy superior to that of placebo with a 52 week glucocorticoid taper in giant cell arteritis.
