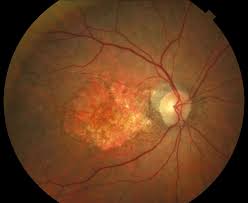
Geographic atrophy (GA), also known as atrophic age-related macular degeneration (AMD) or advanced dry AMD.
It is an advanced form of age-related macular degeneration that can result in the progressive and irreversible loss of retinal tissue: photoreceptors, retinal pigment epithelium, choriocappillaris, which can lead to a loss of visual function over time.
Estimated that GA affects >5 million people worldwide and approximately 1 million patients in the US, which is similar to the prevalence of neovascular (wet) AMD, the other advanced form of the disease.
The incidence of advanced AMD, both geographic atrophy and neovascular AMD, increases exponentially with age and while there are therapies for wet AMD, GA currently has no approved treatment options.
The aim of most current clinical trials is to reduce the progression of GA lesion enlargement.
Geographic atrophy is a chronic disease, which leads to visual function loss, difficulty performing daily tasks such as reading, and driving, and ultimately independence.
Initially, there is good visual acuity if the GA lesions are not involved in the central macular, or foveal, region of the retina.
Standard vision acuity testing may underrepresent the visual deficit experienced by patients who report challenges reading, driving or seeing in low light conditions.
Reading speed is often initially unaffected due to foveal sparing.
Reading speed worsens progressively as the area of atrophy enlarges.
As the disease progresses, vision-related quality-of-life declines markedly.
Fluorescein angiography and optical coherence tomography are established techniques for diagnosing and tracking geographic atrophy.
The pathogenesis of GA is likely multifactorial and triggered by intrinsic and extrinsic stressors to poorly regenerative retinal pigment epithelium (RPE), particularly oxidative stress caused by the high metabolic demand of photoreceptors, photo-oxidation, and environmental stressors such as cigarette smoke.
Variations in several genes, particularly in the complement system, increase the risk of developing GA.
Aging damage caused by these stressors accumulates, which coupled with a genetic predisposition, results in the appearance of drusen and lipofuscin deposits.
These and other products of oxidative stress can trigger inflammation via multiple pathways: complement cascade, ultimately leading to loss of photoreceptors, RPE, and choriocapillaris, culminating in atrophic lesions that grow over time.
Geographic atrophy may be due to deficiencies in blood flow within the choriocapillaris.
Regions of the choriocapillaris which have less blood flow are more likely to degenerate and become geographic atrophy.
The vascular insufficiency hypothesis is supported by non-exudative neovascular membranes, which can recapitulate the choriocapillaris, and associated with a markedly slower GA progression.
Diagnosis:
Fundus autofluorescence and optical coherence tomography angiography are imaging modalities that can be used in the diagnosis.
Optical coherence tomography angiography can help indicate that the patient may be developing wet AMD.
Patients with geographic atrophy are at higher risk for developing advanced wet AMD (neovascular AMD), and can initiate treatment of wet age-related macular degeneration.
Multiple imaging methods can be applied to quantify the area of retinal pigment epithelium atrophy including short-wavelength (blue) fundus autofluorescence imaging, green fundus autofluorescence imaging, and en face optical coherence tomography imaging.
Treatment:
There are currently no approved treatments to reverse or halt the progression of geographic atrophy.
Patients should be regularly followed for development of neovascular AMD, for which that can be treated for that.
