 A rare form of small bowel obstruction caused by an impaction of a gallstone within the lumen of the small intestine.
A rare form of small bowel obstruction caused by an impaction of a gallstone within the lumen of the small intestine.
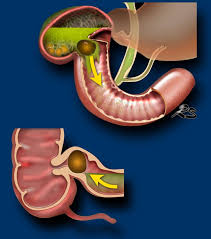
Such a gallstone enters the bowel via a cholecysto-enteric fistula.
A fistula typically develops when inflammation from recurrent episodes of cholecystitis, cause gallbladder adhesions to surrounding organs.
In 85% of patients with gallstone ileus, gallstones travel through a cholecystoduodenum fistula into the duodenum and 15% have a fistula that involves the stomach, small bowel, or transverse colon.
Once gallstones are in the G.I. tract, they typically advance distantly, and are expelled through the rectum, if they are small.
When gallstones have a diameter of 2 cm or greater, they may cause intestinal obstruction, which occurs most commonly in the ileum (50 to 60%) and less frequently in the jejunum, duodenum, colon or stomach.
Large stones, >2.5 cm in diameter, within the gallbladder are thought to predispose to fistula formation by gradual erosion through the gallbladder fundus.
A stone may travel from the gallbladder into the bowel through the fistula and become lodged almost anywhere along the GI tract.
Obstruction occurs most commonly at the near the distal ileum.
Obstruction occurs, usually within 60 cm proximally to the ileocecal valve.
Rarely, gallstone ileus may recur if the underlying fistula is not treated.
Diagnosis requires radiographic studies.
Classic radiographic findings are known as Rigler’s triad of pneumobilia, evidence of small bowel obstruction and radiopaque gallstone on abdominal X-rays.
Diagnosis is often delayed because at least half the patients do not have laboratory abnormalities or history that suggests biliary disease.
The obstructing stone is frequently radiolucent on plane films, complicating the diagnosis.
Patients with gallstone ileus, usually present with nausea, vomiting, abdominal pain, and distention.
Symptoms may be intermittent d gallstones pass along with G.I. tract.
Rarely an impacted gallstone can cause intestinal perforation.
Initial management involves fluid resuscitation and potentially nasogastric suctioning.
It constitutes a form of mechanical small bowel obstruction.
Gall stone ileus represents 1 to 4% of all cases of mechanical G.I. obstruction, and accounts for up to 25% of bowel obstruction in patients older than 65 years.
It generally occurs in older patients with a mean age of 74 years and 80 to 90% of multiple medical conditions, including hypertension, diabetes, and ischemic heart disease.
Between 72 and 90% of patients with gallstone ileus or women.
Approximately 50% of patients with gallstone ileus have no history of gallbladder disease.
It can be a surgical emergency.
It requires open or laparoscopic surgery to remove an impacted stone.
Surgical management may include either enterolithotomy alone, allowing a delayed cholecystectomy after an inflammation-free period of 4–6 weeks or enterolithotomy in combination with a cholecystectomy and fistula division.
Endoscopic removal of the gallstone is possible.
Eecurrent gallstone ileus occurs in approximately 5% of patients treated with enterolithotomy, with 85% of recurrences occurring within six months of surgery.
Gallstone ileus is associated with the mortality rate of 7 to 30%, in part due to the advanced age of patients and their multiple comorbidities.
