 Fetal alcohol syndrome refers to growth, mental, and physical problems that may occur in a newborn when a mother drinks alcohol during pregnancy.
Fetal alcohol syndrome refers to growth, mental, and physical problems that may occur in a newborn when a mother drinks alcohol during pregnancy.
Alcohol easily passes across the placenta to the fetus.
Alcohol should not be consumed while pregnant.
Even a small amount of alcohol is not known to be safe for the unborn baby, as alcohol passes easily from the mother’s bloodstream through the placenta and into the bloodstream of the fetus.
The fetus is smaller and does not have a fully developed liver, the concentration of alcohol in its bloodstream lasts longer, increasing its detrimental side effects.
The effect alcohol may have on a developing fetus depends upon the amount and frequency of alcohol consumed as well as the stage of pregnancy.
Heavy drinking and binge drinking are associated with a higher risk of fetal alcohol spectrum disorders (FASDs).
The most severe form of FASD is fetal alcohol syndrome (FAS).
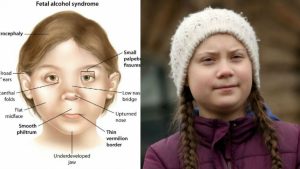
FAS is characterized by slower physical growth, facial abnormalities including smooth philtrum, thin vermilion, and short palpebral fissures, neurological deficits, or smaller head circumference.
It is estimated that nearly 10% of women globally consume alcohol during pregnancy.
About 630,000 infants each year suffer with fetal alcohol spectrum disease, which includes a range of lifelong medical and physical disabilities.
Fetal alcohol spectrum disease refers to patients who experience disability as a result of prenatal alcohol exposure.
Fetal alcohol spectrum disease includes: fetal alcohol syndrome, partial fetal alcohol syndrome, and alcohol related neurodevelopmental disorder.
Estimated there are 3-4 cases of alcohol related neurodevelopmental disorder for every one case of fetal alcohol syndrome.
Every day 100-500 children are estimated to be born with fetal alcohol spectrum disorder in the US.
Fetal alcohol syndrome prevalence estimated to be at least 2-7 cases per 1000 people and prevalence of fetal alcohol spectrum disorder in young school children might be as high as 20-50 cases per 1000 children.
Prevalence of of fetal alcohol spectrum disease is estimated to be at least 10 times higher than the prevalence of fetal alcohol syndrome.
Relatively high prevalence in susceptible populations.
Comorbid conditions for fetal alcohol spectrum disorder include congenital abnormalities, deformities, chromosomal abnormalities, mental and behavioral disorders.
At least as common as autism spectrum disorders.
Costs of care exceeds 3.8 $billion annually.
No safe level of alcohol use during pregnancy has been established.
The expression of fetal alcohol phenotype is age and development dependent.
Larger amounts of alcohol appear to increase problems and binge drinking is more harmful than drinking small amounts of alcohol.
Alcohol is most harmful during the first 3 months of pregnancy, but drinking alcohol any time during pregnancy can be harmful.
A baby with fetal alcohol syndrome may have: poor growth in utero and after birth, decreased muscle tone, poor coordination, delaye development in thinking, speech, movement, or social skills, ventricular septal defect (VSD) or atrial septal defect (ASD), facial abnormalities of narrow, small eyes with large epicanthal folds, microcephaly, small upper jaw, and smooth groove in upper lip.
About one in four patients with fetal alcohol syndrome has either an ASD or a ventricular septal defect.
Delayed or uncoordinated motor skills, hearing or vision problems, learning disabilities, behavior problems, and inappropriate social skills compared to same-age peers are also associated with fetal alcohol spectrum disorder.
Disorder affects CNS and senosry system in 50-90% of children.
Disorders of brain function are the primary processes of prolonged impairments.
Complications seen in the infant may include: impaired in-utero growth, abnormal cardiac structure and function, abnormal head, eyes, nose or mouth structures, developmental impairment, behavior problems, infant death, and mental retardation.
Fetal alcohol spectrum disorder patients are more likely to have trouble in school, legal problems, participate in high-risk behaviors, and develop substance use disorders themselves.
44% of children born to heavy maternal drinkers had functional CNS abnormalities, compared to 13.6% of children who were not exposed to alcohol (Kuehn D et al).
In the above study 27.2% of exposed children had growth restriction compared with 12.5% of the control group, and 17.3% of exposed children had facial abnormalities compared to 1.1% of the control group.
