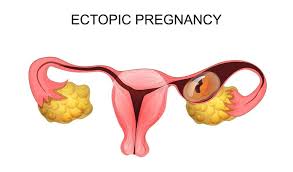
 Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus.
Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus.
Ectopic pregnancy defined as a pregnancy that implants outside of the endometrial cavity, accounts for approximately 2% of all reported pregnancies (CDC).
Frequency about 1.5% of pregnancies,though it may be as high as 4% among those using assisted reproductive technology.
The rate of ectopic pregnancy is about 1% and 2% of that of live births in developed countries, though it is as high as 4% in pregnancies involving assisted reproductive technology.
Ectopic pregnancy is responsible for 6% of maternal deaths during the first trimester of pregnancy.
Also known as eccyesis or tubal pregnancy.
The implantation of a fertilized egg in the fallopian tube is a time sensitive process that can result in tubal rupture and life-threatening hemorrhage.
Hypothesis that tubal ectopic pregnancy is caused by a combination of retention of the embryo within the fallopian tube due to impaired embryo-tubal transport and alterations in the tubal environment allowing early implantation to occur.
An ovarian pregnancy is differentiated from a tubal pregnancy.
Tubal pregnancy at the isthmus or within the uterus, known as interstitial pregnancy, is high as there is increased vascularity that may result in sudden major internal bleeding.
Signs and symptoms of EP include: increased hCG, vaginal bleeding, sudden lower abdominal pain, pelvic pain, a tender cervix, an adnexal mass, or adnexal tenderness.
The symptoms have low specificity, and can be similar to those of other genitourinary and gastrointestinal disorders, such as appendicitis, salpingitis, rupture of a corpus luteum cyst, miscarriage, ovarian torsion or urinary tract infection.
Pain is described as sharp, dull, or crampy, and may also spread to the shoulder if bleeding into the abdomen has occurred.
Severe bleeding may result in shock.
The fetus of ectopic pregnancy is typically not viable.
Rarely, a live baby has been delivered from an abdominal pregnancy.
In abdominal ectopic pregnancy the placenta sits on the intra-abdominal organs or the peritoneum and has found sufficient blood supply.
These sites are generally bowel or mesentery, but other sites, such as the renal, liver or hepatic artery or even aorta have been noted.
An abdominal ectopic pregnancy would have to be delivered by laparotomy.
Cesarean section ectopic pregnancies (CSP) are rare, but are becoming more common.
The incidence of Cesarean section ectopic pregnanciesis not well known: estimates based on different populations of 1:1800-1:2216.
Cesarean section ectopic pregnancies and are characterized by abnormal implantation into the scar from a previous cesarean section.
Cesarean section ectopic pregnancies can cause serious complications such as uterine rupture and hemorrhage.
Cesarean section ectopic pregnancies may present as an asymptomatic process, but symptoms can include vaginal bleeding that may or may not be associated with pain.
Cesarean section ectopic pregnancy diagnosis is by ultrasound.
Ultrasound findings in Cesarean section ectopic pregnancy:
Empty uterine cavity with bright hyperechoic endometrial stripe
Empty cervical canal
Intrauterine mass in the anterior part of the uterine isthmus
Absence of the anterior uterine muscle layer, and/or absence or thinning between the bladder and gestational sac, measuring less than 5 mm.
Management:
Treatment should occur promptly following diagnosis because of the increasing risk for rupture associated for each additional day the process continues.
Cesarean section ectopic pregnancy treatment options: methotrexate or surgical with dilation and curettage, uterine wedge resection, or hysterectomy. Methotrexate administration resulted in successful resolution of the topic pregnancy without further need for surgical intervention from 70 to 95%.
Methotrexate administered intramuscularly is the standard of care for medical management of tubal ectopic pregnancy by inactivating dohydrofolate reductase, which causes depletion of tetrahydrofolate, an essential co-factor for DNA and RNA synthesis so that rapidly dividing cells such as trophoblastic cells are susceptible to its action.
Methotrexate should not be used if pregnancy is desired, eligibility requires an ambulatory setting, hemodynamic stability, no evidence of tubal rupture, and ability to follow up for care.
Serum beta hCG level should be less than 5000 mIU pro, should be absent embryonic cardiac activity, and the size of the ectopic pregnancy less than 4 cm as an alternative to surgical treatment.
Individuals who are not candidates for methotrexate, ie, those with hemodynamic instability, kidney or hepatic dysfunction, active pulmonary disease, heterotopic pregnancy are treated surgically.
The time for pregnancy resolution is about 22 days in cases which medical management was successful; 20% receive a second dose of methotrexate, and 24% undergo surgery.
Ectopic pregnancy is most often treated surgically with laparoscopic removal of the fallopian tube.
Salpingostomy may be considered if there is damage to contralateral fallopian tube and plan for future fertility.
Bilateral salpingectomy is an option for patients who want permanent contraception after treatment of ectopic pregnancy
Other treatments include intragestational methotrexate or potassium chloride injections, intracervical balloon tamponade, nod, and uterine aspiration.
Up to 10% of women with ectopic pregnancy have no symptoms, and one third have no medical signs
Risk factors:
Pelvic inflammatory disease often due to chlamydia infection, tobacco smoking, prior tubal surgery, history of infertility, use of assisted reproductive technology, use of an intrauterine device (IUD), previous exposure to diethylstilbestrol (DES), tubal surgery, intrauterine surgery, previous ectopic pregnancy, endometriosis, previous D&C, and tubal ligation.
The greatest risk factors for EP include: history of pelvic surgery or infection, resulting in disruption of normal fallopian tube anatomy, or a history of a prior ectopic pregnancy.
The risk of ectopic pregnancy increases in individuals with a. Infertility history, as well as those who have conceived by assisted reproductive technology.
Individuals with intrauterine devices have an overall lower risk of pregnancy, yet up to 67% of levonorgestrel IUD users will have an ectopic pregnancy in the event of an unintended pregnancy.
Vaginal douching is possibly related to increased ectopic pregnancies.
Women exposed to DES in utero have an elevated risk of ectopic pregnancy.
Rates of morbidity and mortality due to a EP have racial and age disparities, with mortality rate 6.8 times higher for black pregnant females compared with white pregnant females in the 3.5 times higher risk for individuals older than 35 years compared with those younger than 25 years.
The risk of hemorrhage in untreated ectopic pregnancy is 50% or more.
Approximately 15% of patients with ectopic pregnancy present in hypovolemic shock.
In as many as one third to one half of cases no risk factors can be identified.
Women who have previously had an ectopic pregnancy are at much higher risk of having another one.
Smoking and increased age are risk factors.
In about one half a patients with EP, there is no known risk factor.
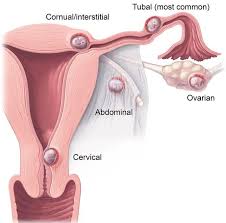
90% of ectopic pregnancies occur in the Fallopian tube which are known as tubal pregnancies.
Implantation can also occur on the cervix, ovaries, or within the abdomen.
Diagnosis is typically by blood tests for human chorionic gonadotropin (hCG) and ultrasound, along with patient, history, and a high index of suspicion.
Any reproductive aged patient presenting with abdominal pain with vaginal bleeding, free fluid on sonogram, and a positive pregnancy test should be tested for ruptured ectopic pregnancy, until proven otherwise.
The primary goal of diagnostic procedures in ectopic pregnancy is to determine risk rather than establishing pregnancy location.
Transvaginal ultrasonography showing a gestational sac with fetal heart in the fallopian tube has a very high specificity of ectopic pregnancy.
Evaluation may require testing on more than one occasion.
Ultrasound works best when performed from within the vagina.
Transvaginal ultrasonography has a sensitivity of at least 90% for ectopic pregnancy.
Ultrasound finding in ectopic pregnancy is an adnexal mass that moves separately from the ovary.
In around 60% of cases of EP, ultrasound finds an inhomogeneous or a noncystic adnexal mass “blob sign”.
The noncystic mass is generally spherical.
The blob sign has been estimated to have a sensitivity of 84% and specificity of 99% in diagnosing ectopic pregnancy.
An empty extrauterine gestational “bagel sign”, is present in around 20% of cases of EP.
In another 20% of cases, there is visualization of a gestational sac containing a yolk sac or an embryo.
Ectopic pregnancies with visualization of cardiac activity are sometimes termed “viable ectopic”.
Prevention is by decreasing risk factors such as chlamydia pelvic infections through screening and treatment.
Some ectopic pregnancies resolve without treatment.
Management includes methotrexate and surgery.
Some ectopic pregnancies will resolve without treatment.
Methotrexate works as well as surgery in some cases.
Methotrexate can be given at the time of surgery prophylactically to prevent persistence of EP.
Methotrexate works well when the beta-HCG is low and the size of the ectopic is small.
Surgery is usually recommended if the tube has ruptured, there is a fetal heartbeat, or there are unstable vital signs.
Rupture of an ectopic pregnancy can lead to abdominal distension, tenderness, peritonism and hypovolemic shock.
Complications:
Rupture with internal bleeding which may lead to hypovolemic shock.
Death from rupture is the leading cause of death in the first trimester of the pregnancy.
A previous induced abortion does not appear to increase the risk.
With an IUD, if pregnancy occurs, it is more likely to be ectopic than intrauterine.
Tubal pregnancy occurs when the egg is implanted in the fallopian tubes.
Surgery can be open or laparoscopic.
The rate of ectopic pregnancy is about 1 and 2% that of live births.
The rate of ectopic pregnancy may be as high as 4% among those using assisted reproductive technology.
EP is the most common cause of death during the first trimester at approximately 10% of the total.
The risk of death from EP in the developed world is between 0.1 and 0.3 percent while in the developing world it is between one and three percent.
Up to 10% of ectopic pregnancies without symptoms, and one-third of cases have no medical signs.
In many the symptoms have low specificity, and can simulate : appendicitis, salpingitis, rupture of a corpus luteum cyst, miscarriage, ovarian torsion or urinary tract infection.
Patients clinically present with EP at a mean of 7.2 weeks after the last normal menstrual period, with a range of four to eight weeks.
Nausea, vomiting and diarrhea are rare symptoms of EP.
Signs and symptoms include: increased hCG, vaginal bleeding, sudden lower abdominal pain, pelvic pain, a tender cervix, an adnexal mass, or adnexal tenderness.
Rupture of an ectopic pregnancy can lead to abdominal distension, tenderness, peritonitis and shock.
As many as one third to one half EP have no risk factors that can be identified.
Previous induced abortion does not appear to increase the risk of EP.
Hypothesis that cilia damage in the Fallopian tubes is likely to lead to an ectopic pregnancy.
Women who smoke have a higher chance of an ectopic pregnancy as it leads to risk factors of damaging and or killing cilia.
Patients with pelvic inflammatory disease (PID) have a high occurrence of ectopic pregnancy, due to scar tissue in the fallopian tubes, causing damage to cilia.
Hair-like cilia located on the internal surface of the fallopian tubes carry the fertilized egg to the uterus: cilia damage in the fallopian tubes is likely to lead to an ectopic pregnancy.
Women who smoke have a higher chance of an ectopic pregnancy in the fallopian tubes, due to damage and killing of cilia by smoking.
With cilia degeneration, the amount of time it takes for the fertilized egg to reach the uterus will increase, and if it doesn’t reach the uterus in time, will hatch from the non-adhesive zona pellucida and implant itself inside the fallopian tube, thus causing the ectopic pregnancy.
Pelvic inflammatory disease (PID) has a high occurrence of ectopic pregnancy, from the build-up of scar tissue in the fallopian tubes, causing damage to cilia.
If both tubes are completely blocked, fertilization of the egg would be impossible, and neither normal pregnancy nor ectopic pregnancy could occur.
Intrauterine adhesions in Asherman’s syndrome can cause ectopic cervical pregnancy or, if adhesions partially block access to the tubes via the ostia, ectopic tubal pregnancy.
Asherman’s syndrome usually occurs from intrauterine surgery, most commonly after D&C.
Tubal ligation can predispose to ectopic pregnancy.
EP risk is higher if a more destructive methods of tubal ligation (tubal cautery) have been used than less destructive methods.
A prior tubal pregnancy increases the risk of future occurrences to about 10%.
Reversal of tubal sterilization carries a risk for ectopic pregnancy.
A history of a tubal pregnancy increases the risk of future occurrences to about 10%.
Advancing age, smoking, exposure to diethylstilbestrol in utero, low socioeconomic status may be associated with ectopic risk.
The diagnosis is considered as the cause of abdominal pain or vaginal bleeding in every woman who has a positive pregnancy test.
The abdominal pain may be described as sharp, dull, or crampy, and may spread to the shoulder if Intraabdominal bleeding has occurred.
A marker of serious intra-abdominal bleeding is the presence of fluid in the hepatorenal recess of the subhepatic space.
An ultrasound examination of a gestational sac with fetal heart in the fallopian tube is highly specificity of ectopic pregnancy, with a sensitivity of at least 90% for ectopic pregnancy.
In around 60% of cases, a noncystic adnexal mass may be seen in case of hematosalpinx.
Ultrasonographic finding is an adnexal mass that moves separately from the ovary.
The US finding of an adnexal mass that moves separately from the ovary has a sensitivity of 84% and specificity of 99% in diagnosing ectopic pregnancy.
The US finding of an empty extrauterine gestational sac is present in around 20% of cases.
In 20% of cases, there is US visualization of a gestational sac containing a yolk sac and/or an embryo.
In fact early pregnancy, ultrasound may be inconclusive and 40% of patients at first evaluation and therefore serial trends in hCG is the standard of care to identify normal and abnormal early pregnancies prior to ultrasound confirmation.
Ectopic pregnancies where there is visualization of cardiac activity are sometimes referred to as viable ectopic.
A positive pregnancy test and the presence of what appears to be a normal intrauterine pregnancy does not exclude an ectopic pregnancy, since there may be either a heterotopic pregnancy or a “pseudosac”, which is a collection of within the endometrial cavity that may be seen in up to 20% of women.
The presence of echogenic fluid in the rectouterine pouch is estimated at between 28 and 56% of women with an ectopic pregnancy, and strongly indicates the presence of hemoperitoneum.
Abdominal EP’s are the only ectopic pregnancies type in which the fetus may rarely survive to term
Doppler ultrasonography is not considered to significantly contribute to the diagnosis of ectopic pregnancy.
A common misdiagnosis is of a normal intrauterine pregnancy is where the pregnancy is implanted laterally in an arcuate uterus.
In the management of a pregnancy of unknown location, that is, a positive pregnancy test but no pregnancy is found on transvaginal ultrasonography.
A low beta-hCG level may indicate that the pregnancy is intrauterine but yet too small to be visible on ultrasonography.
Most consider that the threshold where an intrauterine pregnancy should be visible on transvaginal ultrasound is around 1500 IU/ml of beta-
There is no single threshold for the β-human chorionic gonadotropin that confirms an ectopic pregnancy.
The majority of cases of ectopic pregnancy will have serial serum hCG levels that increase more slowly than would be expected with an IUP, or decrease more slowly than would be expected with a failing PUL.
Up to 20% of cases of ectopic pregnancy have serum hCG doubling times similar to that of an IUP, and around 10% of EP cases have hCG patterns similar to a failing PUL.
There is no single threshold for the beta-human chorionic gonadotropin that confirms an ectopic pregnancy, and the best test in a pregnant woman is a high resolution transvaginal ultrasound.
When there is an adnexal mass in the absence of an intrauterine pregnancy on transvaginal sonography increases the likelihood of an ectopic pregnancy 100-fold.
When there are no adnexal abnormalities on transvaginal sonography, the likelihood of an ectopic pregnancy decreases.
An empty uterus with levels higher than 1500 IU/ml may be evidence of an ectopic pregnancy, but may also be consistent with an intrauterine pregnancy which is simply too small to be seen on ultrasound.
By measuring the beta-hCG level approximately 48 hours later, a fall beta-hCG strongly suggests a spontaneous abortion or rupture.
The majority of cases of ectopic pregnancy will have serial serum hCG levels that increase more slowly than would be expected with an Intrauterine pregnancy.
The majority of cases of ectopic pregnancy will have serial serum hCG levels
that decrease more slowly than would be expected with a failing pregnancy of unknown location.
However, up to 20% of cases of ectopic pregnancy have serum hCG doubling times similar to that of an IUP, and around 10% of EP cases have hCG patterns similar to a failing pregnancy of unknown location.
A laparoscopy can also be performed to visually confirm an ectopic pregnancy, but this procedure is reserved for women presenting with signs of an acute abdomen and/or hypovolemic shock.
Severe bleeding may result in shock.
Culdocentesis, is a less commonly performed test that may be used to look for internal bleeding.
Progesterone levels of less than 20 nmol/l have a high predictive value for failing pregnancies.
Progesterone levels over 25 nmol/l are likely to predict viable pregnancies, and levels over 60 nmol/l are strongly so.
Dilation and curettage is sometimes used to diagnose pregnancy location with the aim of differentiating between an ectopic pregnancy and a non-viable intrauterine pregnancy in situations where a viable IUP can be ruled out.
Dilation and curettage is
sometimes used to diagnose pregnancy location with the aim of differentiating between an EP and a non-viable IUP.
Dilation and curettage indications:
No visible IUP on transvaginal ultrasonography with a serum hCG of more than 2000 mIU/ml.
An abnormal rise in hCG level.
A rise of 35% over 48 hours is proposed as the minimal rise consistent with a viable intrauterine pregnancy.
An abnormal fall in hCG level, such as defined as one of less than 20% in two days.
Ectopic pregnancy is suggested by a failure of beta hCG levels to double in 48 hours or about the development of worsening pain or hemodynamic instability.
Ectopic pregnancies implant primarily in the Fallopian tube.
5% of all ectopic pregnancies grow in the fi burial end of the Fallopian tube,
80% in the ampullary section, the isthmus (12%), and the cornual and interstitial part of the tube (2%).
EPis the most common cause of death among women during the first trimester at approximately 6-13% of the total.
Mortality of a tubal pregnancy at the isthmus or within the uterus is higher as there is increased vascularity that may result more likely in sudden major internal bleeding.
Two percent of ectopic pregnancies occur in the ovary, cervix, or are intraabdominal.
Transvaginal ultrasound examination is usually able to detect a cervical pregnancy.
Very rarely, a live baby has been delivered from an abdominal pregnancy.
In an abdominal pregnancy the placenta sits on the intraabdominal organs or the peritoneum and has found sufficient blood supply.
The diagnosis is most commonly made at 16 to 20 weeks gestation, and such a fetus would have to be delivered by laparotomy
Extrauterine pregnancy morbidity and mortality are high.
Maternal morbidity and mortality from extrauterine pregnancy is high as removing the placenta from the attached organs usually leads to uncontrollable bleeding.
Attempts to remove the placenta from the organs to which it is attached usually lead to uncontrollable bleeding from the attachment site.
If the organ to which the placenta is attached is removable, such as a section of bowel, then the placenta should be removed together with that organ.
The vast majority of abdominal pregnancies require intervention well before fetal viability because of the risk of bleeding.
Heterotopic pregnancy occurs when there may be two fertilized eggs, one outside the uterus and the other inside.
Heterotopic pregnancies are becoming more common, likely due to increased use of IVF.
The survival rate of the uterine fetus of a heterotopic pregnancy is around 70%.
Often the intrauterine pregnancy is discovered later than the ectopic, due tomthe painful emergency nature of ectopic pregnancies.
Heterotopic pregnancies are becoming more common, due to increased use of IVF.
The survival rate of the uterine fetus of an ectopic heterotopic pregnancy is around 70%.
After a conservative procedure that attempts to preserve the affected fallopian tube such as a salpingotomy, in about 15-20% the major portion of the ectopic growth may have been removed, but some trophoblastics tissue can escape removal and continue to grow, generating a new rise in hCG levels.
hCG levels may have to be monitored after removal of an ectopic pregnancy to assure their decline, also methotrexate can be given at the time of surgery prophylactically.
Pregnancy of unknown location (PUL) refers to a pregnancy where there is a positive pregnancy test but no pregnancy has been visualized using transvaginal ultrasonography.
It is estimated that between 8 and 10% of women attending for an ultrasound assessment in early pregnancy will be classified as having a PUL.
The true nature of the pregnancy can be an ongoing viable intrauterine pregnancy, a failed pregnancy, an ectopic pregnancy or rarely a persisting PUL.
In women with a pregnancy of unknown location, between 6% and 20% have an ectopic pregnancy.
Between 30 and 47% of women with pregnancy of unknown location are ultimately diagnosed with an ongoing intrauterine pregnancy.
The majority (50-70%) of women with pregnancy of unknown location are found to have failing pregnancies where the location is never confirmed.
Persisting pregnancy of unknown location is where the hCG level does not spontaneously decline and no intrauterine or ectopic pregnancy is identified on follow-up transvaginal ultrasonography.
Persisting pregnancy of unknown location is likely due to either a small ectopic pregnancy that has not been visualized, or a retained trophoblast in the endometrial cavity.
In women with a pregnancy of unknown location, between 6% and 20% have an ectopic pregnancy.
Between 30% and 47% of women with pregnancy of unknown location are ultimately diagnosed with an ongoing intrauterine pregnancy, whereof the majority (50–70%) will be found to have failing pregnancies where the location is never confirmed.
It is estimated that an acceptable rate of PULs that eventually undergo surgery is between 0.5 and 11%.
Persisting PUL is where the hCG level does not spontaneously decline and no intrauterine or ectopic pregnancy is identified on follow-up transvaginal ultrasonography.
Treatment is considered when a potentially viable intrauterine pregnancy has been definitively excluded.
A PUL is managed medically, generally with methotrexate, without confirmation of the location of the pregnancy.
A resolved persistent PUL is defined as serum hCG reaching a non-pregnant value of less than 5 IU/l) after management, or after uterine evacuation without evidence of chorionic villi on histopathological examination.
A relatively low and unresolving level of serum hCG indicates the possibility of an hCG-secreting tumor.
Differential diagnosis: miscarriage, ovarian torsion, and acute appendicitis, ruptured ovarian cyst, kidney stone, and pelvic inflammatory disease.
The symptoms have low specificity, and can be similar to those of other genitourinary and gastrointestinal disorders, such as appendicitis, salpingitis, rupture of a corpus luteum cyst, miscarriage, ovarian torsion or urinary tract infection.
Expectant management is patients with PUL are followed up with serum hCG measurements and repeat transvaginal examinations until a final diagnosis is confirmed.
Expected management is considered in patients who are hemodynamically stable with a low hCG level, often less than 1000 units and who have declining levels of beta hCG: search man of human should be abandoned if symptoms occur or hCG levels do not decrease.
Persistence of an ectopic pregnancy refers to the continuation of trophoblastic growth after a surgical intervention to remove an ectopic pregnancy.
In about 15–20% of surgically intervened EP, the major portion of the ectopic growth may have been removed, but some trophoblastic tissue, has escaped removal and continues to grow, generating a new rise in hCG levels.
This process may be associated with new clinical symptoms. including bleeding.
hCG levels should be monitored after removal of an ectopic pregnancy to assure their decline.
If bleeding has already occurred, surgical intervention may be necessary.
Surgeons use laparoscopy or laparotomy to gain access to the pelvis and can either incise the affected Fallopian and remove only the pregnancy (salpingostomy) or remove the affected tube with the pregnancy (salpingectomy).
People that undergo salpingectomy and salpingostomy have a similar recurrent ectopic pregnancy rate of 5% and 8% respectively.
Their intrauterine pregnancy rates are also similar, 56% and 61%.
When ectopic pregnancies are treated, the prognosis for the mother is very good in Western countries.
Maternal death is rare, but most fetuses die or are aborted with EP.
In the UK 1 in 3,210 women with an ectopic pregnancy died.
In the developing world, however, especially in Africa, the death rate is very high, and ectopic pregnancies are a major cause of death among women of childbearing age.
In women having had an ectopic pregnancy, the risk of another one in the next pregnancy is around 10%.
Management strategies include surgical, medical or expecting plans.
Surgery is indicated in patients with hemodynamic instability, and who prefer expedited treatment or wish to avoid methotrexate.
Laparotomy for tubal ectopic pregnancy is occasionally warranted in cases of massive intraabdominal hemorrhage or if adhesive disease precludes the laparoscopic approach.
Surgical procedure generally involves either laparoscopic salpingectomy or salpingostomy with removal of the pregnancy through a tubal incision while the tube is preserved, and both can be performed on an outpatient basis.
Early treatment of an ectopic pregnancy with methotrexate is a viable alternative to surgical treatment.
If administered early in the pregnancy, methotrexate terminates the growth of the developing embryo.
Methotrexate may cause an abortion, or the developing embryo may then be either resorbed or passed with a menstrual period.
Contraindications to methotrexate use include liver, kidney, or blood disease, as well as an ectopic embryonic mass > 3.5 cm.
Use of methotrexate may lead to the inadvertent termination of an undetected intrauterine pregnancy, or severe abnormality in any surviving pregnancy.
Methotrexate usage recommended only when hCG has been serially monitored with a rise less than 35% over 48 hours, which practically excludes a viable intrauterine pregnancy.
Methotrexate administered intramuscularly is the standard of care for medical management of tubal ectopic pregnancy.
Methotrexate in activates dihydrofolate reductase depleting tetra hydrofolate, an essential cofactor for DNA and RNA synthesis: rapidly dividing cells, such as a trophoblastic cells are susceptible to its action.
The United States uses a multi dose protocol of methotrexate (MTX) which involves 4 doses of intramuscular along with an intramuscular injection of folinic acid to protect cells from the effects of the drugs and to reduce side effects.
Dose schedules include single dose, two dose or multiple dose protocols.
Eligibility for medical management includes: hemodynamic stability, no evidence of tubular rupture, and ability to follow up for care, no difficulty following the patients beta hCG level, bea hCG level less than 5000 international units, absent embryonic cardiac activity, and the size of ectopic pregnancy of less than 4 cm.
Methotrexate terminates the growth of the developing embryo, may cause an abortion, or the developing embryo may then be either resorbed by the woman’s body or pass with a menstrual period.
The median time to pregnancy resolution with methotrexate is around 28 days.
Contraindications to methotrexate include liver, kidney, or blood disease, as well as an ectopic embryonic mass > 3.5 cm.
Methotrexate may lead to the inadvertent termination of an undetected intrauterine pregnancy, or severe abnormality in any surviving pregnancy, and should only be administered when hCG has been serially monitored with a rise less than 35% over 48 hours, which practically excludes a viable intrauterine pregnancy.
Using laparoscopy or laparotomy to gain access to the pelvis the affected Fallopian tube can be removed, or the pregnancy can removed.
Rates of intrauterine pregnancy two years after treatment of ectopic pregnancy are approximately 64% with radical surgery, 67% with medication, and 70% with conservative surgery.[63] In comparison, the cumulative pregnancy rate of women under 40 years of age in the general population over two years is over 90%.[64]
Methotrexate does not affect future fertility treatments.
The number of oocytes that can be retrieved before and after treatment with methotrexate does not change.
In case of ovarian ectopic pregnancy, the risk of subsequent ectopic pregnancy or infertility is low.
The rate that PULs that eventually undergo surgery is between 0.5 and 11%.
The most common complication of ectopic pregnancy is rupture with internal bleeding.
Death from rupture is still the leading cause of death in the first trimester of the pregnancy.
Prognosis: Mortality 0.2% and 2% in the developing world.
Mortality 3.5 times higher risk for individuals older than 35 years compared with those younger than 25 years.
In the developing world the death rate is very high, and ectopic pregnancies are a major cause of death among women of childbearing age.
The rates of intrauterine pregnancy 2 years after treatment of ectopic pregnancy are approximately 64% with radical surgery, 67% with medication, and 70% with conservative surgery.
The cumulative pregnancy rate of women under 40 years of age in the general population over 2 years is over 90%.
The rate of ectopic pregnancy is about 1 and 2% of that of live births in developed countries, though it is as high as 4% in pregnancies involving assisted reproductive technology.
Between 93 and 97% of ectopic pregnancies are located in a Fallopian tube.
Ectopic pregnancies can grow in the fimbrial end (5%) , the ampullary section (80%), the isthmus (12%), and the cornual and interstitial part of the tube (2%).
Ectopic pregnancy is responsible for 6% of maternal deaths during the first trimester of pregnancy making it the leading cause of maternal death during this stage of pregnancy.
There have been cases where ectopic pregnancy ended in a live baby delivered by laparotomy.
Prevention: decreasing risk factors such as chlamydia infections through screening and treatment.
