 A right heart disorder with malformation of the right ventricle and tricuspid valve, including the downward displacement of the tricuspid leaflets and abnormalities of the distal attachments of the tricuspid valve.
A right heart disorder with malformation of the right ventricle and tricuspid valve, including the downward displacement of the tricuspid leaflets and abnormalities of the distal attachments of the tricuspid valve.
A rare congenital heart defect in which the tricuspid valve does not delaminate completely from the underlying myocardium during gestational development.
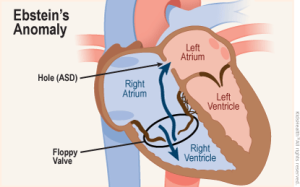
A congenital heart defect in which the septal leaflet of the tricuspid valve is displaced towards the apex of the right ventricle of the heart.
Marked by malformations of the tricuspid valve and right ventricle.
The degree of incomplete delamination is variable and the clinical significance ranges from a critically ill newborn to an incidental finding of cardiomegaly on chest x-ray in an asymptomatic adult.
The annulus of the valve is in the normal position, but the valve leaflets are attached to the walls and septum of the right ventricle, to a varying degree.
A portion of the right ventricle is contiguous with the right atrium causing the right atrium to be large and the anatomic right ventricle to be small in size.
There is displacement of the septal leaflet toward the apex, a billowing anterior leaflet, and areas of tethering restricting leaflet motion resulting in severe tricuspid regurgitation with different degrees of right ventricular enlargement and dysfunction.
There is an enlargement of the aorta in 1 out of 200,000 live births.
Displacement of the tricuspid valve towards the apex of the right ventricle is often associated with other abnormalities.
Usually anatomic abnormalities of the tricuspid valve, with enlargement of the anterior leaflet of the valve and other leaflets are plastered to the endocardium.
Septal and posterior leaflets of the tricuspid valve can be fixed to underlying myocardium .
The anterior leaflet of the tricuspid valve can be redundant, tethered or fenes treated.
Functional tricuspid annulus occupies a lower position in the right ventricle so part of the chamber is atrialized or adjoins the right atrium dilating the right atrium.
About 50% of individuals with Ebstein anomaly have an associated shunt between the right and left atria: either atrial septal defect or a patent foramen ovale.
About 50% of individuals with Ebstein anomaly have Wolff-Parkinson-White syndrome, due to the atrialized right ventricular tissue.
EKG changes include right atrial enlargement or tall and broad P waves, first degree atrioventricular block manifesting as a prolonged PR-interval, low amplitude QRS complexes in the right precordial leads, atypical right bundle branch block, T wave inversion in V1-V4 and Q waves in V1-V4 and II, III and aVF.
Typically presents as an AV reentrant tachycardia with associated pre-excitation.
About 30% of patients have an accessory AV pathway.
Beta blockers, calcium channel blockers and digoxin are contraindicated, as AV-blockade may promote conduction over the accessory pathway.
The major determinants of the hemodynamic difficulties related to the distortion of the anterosuperior leaflet of the tricuspid valve and the degree of right ventricle atrialization.
Based on the multiple right sided abnormalities, the severity, clinical pattern, and options for repair vary.
While left heart anomalies are reported infrequently in this abnormality left ventricular dysfunction secondary the paradoxical ventricular septal motion defects, incidental mitral valve disease , endocardial fibrosis and rarely myocardial infarction may be seen.
Abnormalities of the left ventricle cavity, its contour and contractibility reported in as many as 67% of patients.
In a study of 106 consecutive patients with Ebstein anomaly (Jost et al.) the left ventricle was noted to be abnormal frequently with myocardial changes resembling mild noncompaction, and aortic and mitral valve abnormalities were more common than in the general population.
Jost found other abnormalities including left ventricle noncompaction, bicuspid aortic valves (8%), ventricular septal defects (8%) and mitral valve abnormalities were seen in 39% of patients.
Left ventricular noncompacted myocardium seen in almost 18/% of patients.
The management is difficult due to the combination of a severely dilated and dysfunctional right ventricle making valve replacement risky.
Surgical intervention for the following indications:limited exercise capacity (NYHA III-IV), increasing heart size (cardiothoracic ratio greater than 65%), cyanosis (resting oxygen saturation of less than 90%), tricuspid regurgitation with symptoms, paradoxical embolism, transient ischemic attack progressive right ventricular dilation, reduction in right ventricular systolic function, or stroke.
At times the valve tissue is very tenuous with marked fragility defying the ability to hold sutures.
The valve may be rolled, dysplastic, and unable to be moved.
Attempts should be made to preserve the native tricuspid valve.
Surgical intervention involves repair or replacement of the tricuspid valve as well as concomitant atrial septal defect closure if present.
