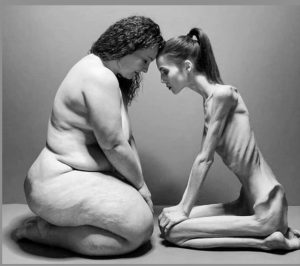
 Most common psychiatric problem of young women.
Most common psychiatric problem of young women.
Eating disorders affect approximately 4. 9% of the women and 2.2% of men in the US.
Globally, eating disorders affect 2 to 5% of individuals during their lifetime and are more common in females than males.
Estimated lifetime prevalence is for anorexia nervosa, bulimia nervosa, and binge eating disorder in adult women are 1.42%, 0.46%, and 1.25%, respectively, and are lower in adult men with anorexia, 0.12%, bulimia nervosa .08%, and binge eating disorder 0.42%.
Binge eating disorder, bulimia nervosa and anorexia nervosa are estimated to affect approximately 1.5 million, 500,000, and 175,000 adults in the US, respectively.
Eating disorder prevalence ranges from 0. 3% to 2. 3% in adolescent females and 0. 3% to 1.3% in adolescent males.
Eating disorders have both genetic and environmental risk factors.
Risk factors for developing an eating disorder include: family history, childhood maltreatment, such as emotional, physical or sexual abuse, although many individuals with EDs have none of these risk factors.
Malnutrition and life stresses arising from gestation through adolescence may interact with genetics susceptibility and development of ED‘s.
Economic cost of eating disorders in the US due to medical care and loss of workplace productivity was estimated to be $65 billion in 2018 to 2019.
Psychiatric comorbidity extremely common.
Occurs most commonly in adolescents and young adults and are 10 times more common in females.
Eating disorders occur more frequently among females than males: 12 to one ratio for anorexia nervosa, 5.8:1 for bulimia nervosa and 3:1 for a binge eating disorder.
Principal disorders are increased in patients who have the severest disorders.
Patient with eating disorders may transition to different eating disorders: 16.8% of patients followed over six years transitions from anorexia nervosa to bulimia nervosa.
Dysregulation of appetite lies at the root of anorexia nervosa, bulimia nervosa, and binge eating disorder.
Eating disorders occur with other psychiatric disorders include mood disorders, anxiety, disorders, obsessive compulsive, disorder, and substance abuse disorders, such as alcohol and stimulant use.
A comprehensive evaluation for psychiatric and substance use disorders is recommended for patients with eating disorders.
Strongly associated with mood and anxiety disorders.
Eating disorders are associated with short term and long term adverse health outcomes including: physical, psychological, and social problems.
Psychiatric comorbidity, and suicidal or self harm ideation and comorbid illness increased risk of death with eating disorders.
A metaanalysis suggested the weighted crude mortality rate for anorexia nervosa was 5.1 deaths per 1000 person-years, and the overall mortality ratio for anorexia nervosa (observed deaths among affected individuals to expected deaths in the general population) was 5.86.
Seen in individuals with low self-esteem, perfectionists, and unable to express negative emotions.
Common among type I diabetic young women.
Hyperthyroidism, inflammatory disease, malignancy, diabetes, chronic infections, Addison’s disease must be considered before the diagnosis is made.
Lifetime risk of major depression 80%.
Frequently progress to chronic illnesses leading to long term treatment and multiple hospitalizations.
Starvation and purging initially calm feelings of anxiety and reduce of obsessions and compulsions by a serotonergic neuronal pathway.
There is a low rate of help- seeking behavior in patients with anorexia nervosa (34.5%), bulimia nervosa (62.6%), and binge eating disorder (49%).
Men and ethnic/racial minorities are significantly less likely to seek help than women and white individuals.
