 Other names include Conjugated Hyperbilirubinemia.
Other names include Conjugated Hyperbilirubinemia.
Symptoms-Jaundice, otherwise asymptomatic.
Dubin–Johnson syndrome is a rare, autosomal recessive, benign disorder that causes an isolated increase of conjugated bilirubin in the serum.
It is due to a defect in the multiple drug resistance protein 2 gene (ABCC2), located on chromosome 10.
It is likely due to a loss of function mutation, since the mutation affects the cytoplasmic/binding domain.
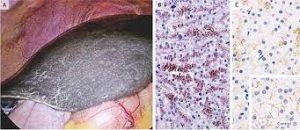
Dubin–Johnson syndrome, causes a black liver due to the deposition of a pigment similar to melanin.
It is associated with a defect in the ability of hepatocytes to secrete conjugated bilirubin into the bile, and is similar to Rotor syndrome.
The conjugated hyperbilirubinemia is a result of defective endogenous and exogenous transfer of anionic conjugates from hepatocytes into bile.
Impaired biliary excretion of bilirubin glucuronides is due to a mutation in the canalicular multiple drug-resistance protein 2 (MRP2).
A darkly pigmented liver is due to polymerized epinephrine metabolites, not bilirubin.
It is usually asymptomatic.
May be diagnosed in early infancy based on laboratory tests.
No treatment is usually needed.
Around 80 to 99% of people with Dubin-Johnson syndrome have jaundice, dark urinary color, biliary tract abnormality, and conjugated bilirubinemia.
Around 30 to 79% of patients with Dubin–Johnson syndrome disorder have abnormality of the gastric mucosa.
Rare symptoms include fever and fatigue.
DIAGNOSIS:
A hallmark is the unusual ratio between the byproducts of heme biosynthesis.
Normal subjects have a coproporphyrin III to coproporphyrin I ratio around 3–4:1.
With Dubin–Johnson syndrome, this ratio is inverted, with coproporphyrin I being 3–4 times higher than coproporphyrin III.
There is a normal level of coproporphyrin in the urine,but the I isomer accounts for 80% of the total, which is normally 25%).
For the first two days of life neonates have ratios of urinary coproporphyrin similar to those seen in patients with Dubin–Johnson syndrome; by 10 days of life, however, these levels convert to the normal ratios.
The liver appears have a dark pink or black appearance due to pigment accumulation.
Dubin–Johnson syndrome is similar to Rotor syndrome, but can be differentiated by:
Rotor syndrome vs Dubin–Johnson syndrome:
Appearance of liver normal histology and appearance vs liver has black pigmentation in D-J sx.
Gallbladder visualization gallbladder can be visualized by oral cholecystogram- gallbladder cannot be visualized in D-J sx.
Total urine coproporphyrin content is high with <70% being isomer 1 and normal with >80% being isomer 1 (normal urine contains more of isomer 3 than isomer 1).
A test of MRP2 activity can also be done to differentiate between Dubin–Johnson syndrome and Rotor syndrome: In case of Dubin–Johnson syndrome, clearance of bromsulphthalein will be within 90 minutes, while in case of Rotor syndrome, the clearance is slow, takes more than 90 minutes for clearance.
Dubin–Johnson syndrome is a benign condition and no treatment is required.
Prognosis is good, and treatment of this syndrome is usually unnecessary.
Most patients are asymptomatic and have normal lifespans.
Some neonates present with cholestasis.
Hormonal contraceptives and pregnancy may lead to overt jaundice and icterus (yellowing of the eyes and skin).
