 Magnified view of the cervix performed to identify and biopsy pre-invasive lesions of cervical intraepithelial neoplasia.
Magnified view of the cervix performed to identify and biopsy pre-invasive lesions of cervical intraepithelial neoplasia.
It is the primary method were evaluating women with abnormal cervical cytology.
The main goal of colposcopy is to prevent cervical cancer by detecting and treating precancerous lesions early.
Other reasons for a patient to have a colposcopy include assessment of diethylstilbestrol (DES) exposure in utero, immunosuppression, abnormal appearance of the cervix or as a part of a sexual assault forensic examination.
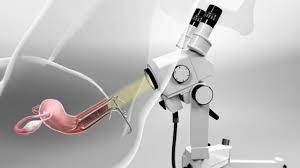
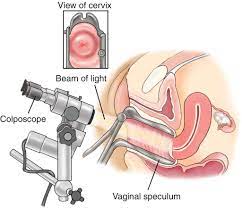
The cervix is viewed through a long focal-length dissecting microscope.
Colposcopy is done using a colposcope, which provides a magnified and illuminated view of the areas, allowing the colposcopist to visually distinguish normal from abnormal appearing tissue, such as damaged or abnormal changes in the tissue, and take directed biopsies for further pathological examination if needed.
A 4% solution of acetic acid is applied to the cervix before viewing, and coloration induced by the acid and the appearance of blood vessel patterns allow a directed biopsy to rule out invasive disease and to determine the extent of preinvasive disease of the cervix.
If entire squamo-columnar junction of the cervix is visualized endocervical curettage is not necessary.
Transformed cells that become pre-cancerous clones, often form laterally spreading high-grade lesions, visible as acetowhite plaques on colposcopy.
Colposcopic magnification with the ancetic acid staining of the cervical transition zone may reveal thickened white epithelium, and vascular markings, suggested of dysplasia or microinvasion.
Typically 2 to 4 biopsies are performed in acetowhite areas.
Colposcopy is not generally performed for people with pap test results showing low-grade squamous intraepithelial lesion (LSIL) or less.
Unless the person has a visible lesion, colposcopy for this population does not detect a recurrence of cancer.
A colposcope is used to identify visible clues suggestive of abnormal tissue.
A lighted binocular or monocular microscope magnifies the view of the cervix, vagina, and vulvar surface.
The squamocolumnar junction, or “transformation zone”, is the critical area on the cervix where many precancerous and cancerous lesions most often arise, and the ability to see the transformation zone and the entire extent of any lesion visualized determines whether an adequate colposcopic examination is attainable.
Acetic acid solution is applied to the surface of the cervix improves visualization of abnormal areas.
Areas of the cervix that turn white after the application of acetic acid or have an abnormal vascular pattern are considered for biopsy.
The colposcopist may obtain biopsies from these areas.
Most doctors and patients consider anesthesia unnecessary.
The use a topical anesthetic such as lidocaine or a cervical block to decrease patient discomfort, particularly if many biopsy samples are taken is considered.
Following any biopsies, an endocervical curettage is often done to simultaneously collect tissue, or a cytobrush to scrape the inside of the cervical canal.
Locations of colposcopy findings can be described in terms of quadrants, or corresponding to a clock face.
Findings are scored based on different parameters and indicate the necessity of biopsy.
Complications from a colposcopy are not common but may include bleeding, infection at the biopsy site or endometrium, and failure to identify the lesion.
Colposcopy with biopsy does not cause infertility or subfertility.
Colposcopic biopsy results are reported using for Bethesda system as CIN1,2.3 or squamous terminologies LSIL or HSIL.
LSIL approximately corresponds to CIN1 and histologic HSIL to CIN2 and CIN3.
CIN3 is more likely to correlate with cellular transformation and risk for progression to cancer who is associated with highly questionable carcinogenic HPV genotypes.
Treatment is recommended for all non-pregnant individuals with a diagnosis of CIN3, or histological HSIL.
Treatments for significant lesions include ablative treatments (cryotherapy, thermocoagulation, and laser ablation) and excisional methods (loop electrosurgical excision procedure or LEEP, or Cervical conization).
