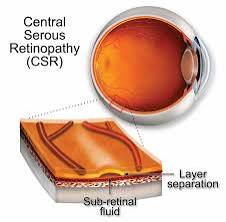
 Central serous retinopathy (CSR) is an eye disease that causes visual impairment, often temporary, usually in one eye.
Central serous retinopathy (CSR) is an eye disease that causes visual impairment, often temporary, usually in one eye.
It has an incidence of 9,9 per 100.000 in men and 1,7 per 100.000 in women, and is the fourth most common retinal disorder.
It is characterized by leakage of fluid under the retina that has a propensity to accumulate under the central macula.
It results in blurred or distorted vision.
The reduced visual acuity may persist after the fluid has disappeared.
The disease is considered of unknown cause.
Mostly affects white males in the age group 20 to 50.
It has a male:female ratio 6:1.
The condition is believed to be exacerbated by stress or corticosteroid use.
In CSR the highly vascularized layer below the retina, is thickened and congested with increased blood vessel diameter, especially in the deep choroid.
This results in increased pressure from the deep choroid against the superficial choroid close to the retina, damaging the fine capillary blood vessels needed to supply oxygen and nutrients to the retinal pigment epithelium and retina.
Fluid can leak from these damaged vessels and accumulate under the retina.
Different stages are defined depending on the amount of cumulative damage.
Accumulation of fluid results in central serous chorioretinopathy (CSR).
The development of secondary blood vessels, so-called choroidal neovascularization (CNV) leads to pachychoroid neovasculopathy (PNV).
Bulging of these new vessels, aneurysms, develop within this CNV, defining pachychoroid aneurysmal type 1 CNV/or, polypoidal choroidal vasculopathy (PCV).
Pachychoroidal diseases of the macula are divided into 4 stages.
Pachychoroid spectrum disorders of the macula:
0 Uncomplicated pachychoroid (UCP)
I Pachychoroid pigmentepitheliopathy (PPE)
II Central serous chorioretinopathy (CSC)
III Pachychoroid neovasculopathy (PNV)
a) with neurosensory detachment (subretinal fluid)
b) without neurosensory detachment (no subretinal fluid)
IV Pachychoroid aneurysmal type 1 choroidal neovascularization (PAT1)
(also polypoidal choroidal vasculopathy, PCV)
CSR is sometimes called idiopathic.
Stress appears to play an important role, in that persons in stressful occupations, such as airplane pilots, have a higher incidence of CSR.
CSR has also been associated with cortisol and corticosteroids.
Corticosteroids commonly used to treat inflammations, allergies, skin conditions and even certain eye conditions, can trigger CSR, aggravate it and cause relapses.
People who have irregular sleep patterns, type A personalities, sleep apnea, or systemic hypertension are more susceptible to CSR: thought to be elevated circulating cortisol and epinephrine, which affect the autoregulation of the choroidal circulation.
Evidence that helicobacter pylori as plays a role, as the presence of the bacteria is well correlated with visual acuity and other retinal findings following an attack.
Evidence also shows that people with glomerulonephropathy type II kidney disease can develop retinal abnormalities including CSR caused by deposits of the same material that originally damaged the glomerular basement membrane in the kidneys.
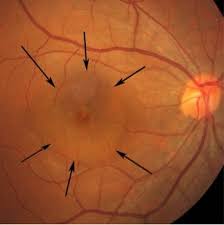
Optical coherence tomography imaging of central serous retinopathy is diagnostic.
The diagnosis usually starts with a dilated examination of the retina, followed with confirmation by optical coherence tomography and fluorescein angiography.
The angiography test Y show one or more fluorescent spots with fluid leakage.
In 10%-15% of the cases these will appear in a smokestack shape.
Differential diagnosis shouldrule out retinal detachment, which is a medical emergency.
Indocyanine green angiography or laser Doppler imaging can be used to reveal the underlying swollen choroidal vessels under the retinal pigment epithelium.
Management:
Any ongoing corticosteroid treatment should be tapered and stopped, where possible.
Most eyes with CSR undergo spontaneous resorption of subretinal fluid within 3–4 months, and recovery of visual acuity usually follows.
Treatment should be considered if resorption does not occur within 3–4 months.
Photodynamic therapy is the treatment of choice for CSR with subretinalfluid for longer than 3–4 months.
Photodynamic therapy (PDT) with verteporfin has efficacy, and long-term effectiveness.
Indocyanine green angiography can be used to predict how the patient will respond to PDT.
Laser photocoagulation,can burnthe leak area shut, is considered in cases where there is little improvement in a 3- to 4-month duration, and the leakage is confined to a single or a few sources of leakage at a safe distance from the fovea.
Laser photocoagulation is not indicated for cases where the leak is very near the central macula or where the leakage is widespread.
Spironolactone is a mineralocorticoid receptor antagonist that may help reduce the fluid associated with CSR.
Eplerenone is another mineralocorticoid receptor antagonist that has been thought to reduce the subretinal fluid that is present with CSR.
Low dosage ibuprofen has been shown to quicken recovery in some cases.
No topical treatment has been proven to be effective in the treatment of CSR.
With management of stressful lifestyle patterns and associated cortisol and epinephrine levels, it has been shown that the fluid associated with CSR can spontaneously resolve.
Melatonin has been shown to help regulate sleep in people who have irregular sleep patterns can better regulate cortisol and epinephrine levels to manage CSR.
Micropulse laser treatments, where patients with acute and chronic CSR had improved visual acuity compared to control patients.
The prognosis for CSR is excellent.
Over 90% of patients regain 20/25 vision or better within 45 days.
Once the fluid has resolved, some visual abnormalities can remain even where visual acuity is measured at 20/20, and
includes localized reductions in light sensitivity as assessed by visual field testing, decreased night vision, reduced color discrimination, and localized distortion caused by scarring of the sub-retinal layers.
Complications of CSR include subretinal neovascularization and pigment epithelial detachment.
CSR can re-occur causing progressive vision loss.
A chronic form, titled as type II central serous retinopathy, occurs in approximately 5% of cases.
Type II central serous retinopathy
exhibits diffuse rather than localized abnormality of the pigment epithelium, producing a persistent subretinal fluid.
The prognosis for this condition is less favorable.
