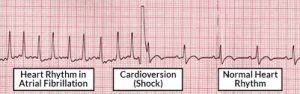
 Cardioversion is a medical procedure by which a tachycardia or cardiac arrhythmia is converted to a normal rhythm, using electrical current or drugs.
Cardioversion is a medical procedure by which a tachycardia or cardiac arrhythmia is converted to a normal rhythm, using electrical current or drugs.
Synchronized electrical cardioversion uses a therapeutic dose of electric current to the heart, at a specific moment in the cardiac cycle.
Synchronized cardioversion is a medical procedure commonly used to treat certain types of abnormal heart rhythms, particularly atrial fibrillation and atrial flutter.
During synchronized cardioversion, an electrical shock is delivered to the heart in a controlled manner to help restore a normal heart rhythm.
synchronized term refers to the timing of the electrical shock with the heart’s natural electrical activity.
By synchronizing the delivery of the electrical shock with a specific phase of the heart’s electrical cycle, usually the R wave on the ECG, synchronized cardioversion can help prevent the induction of dangerous heart rhythms, such as ventricular fibrillation.
Pharmacologic cardioversion, also called chemical cardioversion, uses antiarrhythmia medication instead of an electrical shock.
Synchronized electrical cardioversion utilizes two electrode pads or, alternatively, the traditional hand-held paddles, made up of a metallic plate which is faced with a saline based conductive gel.
The pads are placed on the chest, or one is placed on the chest and one on the back, and these are connected by cables to an ECG display screen and a defibrillator.
The cardioverter has a synchronizer that delivers a reversion shock, of a selected amount of current over a predefined number of milliseconds at the optimal moment in the cardiac cycle corresponding to the R wave of the QRS complex.
The proper timing of the shock at the R wave prevents shock from occurring during the vulnerable period of the cardiac cycle, which could induce ventricular fibrillation.
In a conscious patient, in an elective procedure drugs are often used to help sedate the patient.
Iin hemodynamically unstable or unconscious patients, the shock is given immediately upon confirmation of the arrhythmia.
Synchronized electrical conversion shocks can be performed in conjunction with drug therapy until sinus rhythm is attained.
Synchronized electrical cardioversion is used to treat hemodynamically significant supraventricular tachycardias, including atrial fibrillation and atrial flutter, and wide complex tachycardias, including ventricular tachycardia, when a pulse is present.
Pulseless ventricular tachycardia and ventricular fibrillation are treated with unsynchronized shocks referred to as defibrillation.
Electrical therapy is inappropriate for sinus tachycardia.
Pharmacological cardioversion is an especially good option in patients with fibrillation of recent onset.
Drugs that are effective at maintaining normal rhythm after electric cardioversion include: amiodarone, diluting azem, verapamil, and metoprolol.
These same agents can also be used for pharmacological cardioversion.
Use of heparin plus transesophageal echocardiography to rule out left atrial thrombus can speed time to cardioversion.
Current guidelines recommend anticoagulation for a minimum of 3 weeks before cardioversion and 4 weeks after cardioversion.
In a randomized trial, patients with atrial fibrillation undergoing elective cardioversion were randomized to either rivaroxaban or warfarin and both agents appeared to be equally safe.
In a randomized trial of 1504 patients with atrial fibrillation and cardioversion this agent was safe and effectively prevented the risk of stroke (Cappato R et al).
In the above study Rivaroxaban’s 2-4 hour action allows for a more rapid conversion than vitamin K antagonists.
The cumulative incidence risk in the above study for composite outcome of stroke, non-CNS embolism, TIA, myocardial infarction, and all- cause mortality was 0.61% with Rivaroxaban and 1.22% in patients receiving vitamin K antagonists.
