 The CNS (central nervous system) is affected by a large number of primary brain tumors and by metastases of cancers originating from other organs.
The CNS (central nervous system) is affected by a large number of primary brain tumors and by metastases of cancers originating from other organs.Approximately 17,000 primary central nervous system malignant tumors diagnosed each year.
Generalized headache or unilateral throbbing may be accentuated after supine positioning, in the morning, and improved when upright during the day.
Prevalence studies estimated that there were 138,054 patients with a diagnosis of the primary malignant brain tumor in the US in 2010.
Approximately 13,000 deaths per year in the U.S.
Malignant ((glioma))s are the most common type of primary malignant brain tumor, accounting for 80% of patients in the annual incidence of 5.26 per 100,000 population or 17,000 new cases a year.
5-year survival rates for malignant brain tumors are the third lowest among all types of cancer.
Prognosis depends on locale of the tumor, but more importantly on the histology.
Commonly have different grades within one brain lesion specimen.
Primary and metastatic tumors have significant areas of hypoxia which is associated with poorer prognoses.
Approximately 60% of primary CNS tumors are gliomas with about 65% high-grade Grade III and Grade IV lesions.
In children under the age of 15 years 5-year survivals are 73.3%.
5-year survival rate for children with low-grade cystic cerebeller astrocytomas greater than 90%.
5-year survival rate for children with high-grade diffuse brainstem gliomas is less than 10%.
Incidence of primary tumors of the central nervous system about 11 per 100,000 persons per year.
Most common symptoms include headache, nausea, vomiting, anorexia, dizziness, drowsiness, focal neurological deficits determined by size and site of the tumor and can affect motor/sensory functions.
Headaches occur in 60% of patients who have a brain tumor.
Seizures may occur in up to 50% of patients.
Cognitive impairment and personality changes may occur.
Headaches are usually made worse by the Valsalva maneuver, and upon awakening, reflecting increases in intracranial pressure.
Headaches may be associated with papilledema, focal neurologic abnormalities, nausea or seizures.
Ionizing radiation only unequivocal risk factor identified for glial and meningeal neoplasms.
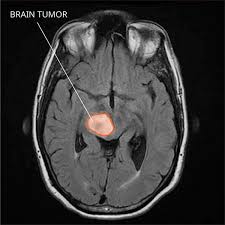
Test of choice for diagnosis is and MRI of the brain with gadolinium enhancement.
A normal contrast-enhanced MRI scan essentially rules out the possibility of a brain tumor.
Glioblastomas typically show contrast enhancement on T1-weighted sequences;T2 – weighted/fluid-attenuated inversion recovery (T2/flare) reveals hyperintense cerebral edema; Central necrosis, and signs of local mass effect may also be present.
Lower grade gliomas are often hypodense on T1 weighted imaging and hyperintense on T2/flare.
Primary CNS lymphoma may be multifocal and demonstrate homogeneous enhancement and fusion restriction on the fusion, weighted imaging.
Glial tumors-histological features of the tumor and the patient’s age and performance status are major prognostic factors and have more influence than any specific therapy on the outcome.
Cognitive defects shortly after radiation therapy are due to deficits present before treatment and are probably caused by the disease itself.
Cognitive impairment associated with primary or metastatic lesions of the brain and from treatments, including radiation, occurs in 10% of patients developing progressive dementia and 50-90% showing cognitive deficits by sensitive testing.
Only one third of children with benign brain tumors treated with surgery alone survive without neurological deficits.
Prophylaxis against seizures with antiepileptic drugs is not supported by the literature.
Antiepileptic drugs are used with caution in brain tumor patient’s because of multiple potentially serious interactions with chemotherapy or corticosteroids (Glantz MJ).
The use of glucocorticoids improved edema, mass effect and decrease his contrast enhancement, and these changes may be related to the induction of vasoconstriction and reduction in vascular permebility (Piette C, Jarden JO, Leenders KL).
The use of steroids in patients with brain tumors should be limited to those with symptomatic mass effect or cerebral edema.
Dementia may occur in children below the age of 2 years that have been treated with cranial or craniospinal radiation.
Children treated for brain tumors are 10.8 times less likely to be employed and 28.8 times less likely to be able to drive a car than their non-treated siblings.
Cognitive problems in children appear 2 or more years after completion of treatment.
Tumor tissue is required to establish the diagnosis.
Procedures are typically performed under general anesthesia and preservation of neurologic function with maximal safe surgical resection is a priority.
Patients may undergo awake craniotomies with repetitive neurologic assessment during the resection.
When esection is not feasible, a tumor biopsy is performed.
Accurate grading of CNS tumors can estimate patient prognosis and requires integration of histological features and molecular abnormalities.
Molecular testing is required to diagnose subtypes of glioma with characterization by specific molecular alterations.
Astrocytomas with mutations of IDH 1 or IDH 2 and homozygous loss of cyclin dependent kinase, inhibitor 2A and B, are considered grade 4, even if they lack histological features of a grade 4 tumor.
Patients with ependymomas require craniospinal MRI and CSF cytology following surgery to assess for leptomeningeal dissemination.
Seizures occur in as many as 75% of patients with glioma.
Non-enzyme inducing anti-elliptic agents such as levetiracetam, lacosamide or clobazam are preferred due to fewer drug to drug interactions and improved adverse effect profiles.
Cerebral edema is treated corticosteroids with dexamethasone being preferred due to its low minerocorticoid activity and long half-life.
Bevacizumab monoclonal body against the vascular endothelia growth factor A can improve cerebral edema in patients with brain tumors who do not respond to steroids or who are intolerant intolerant to steroids.
For treatment recommendations see articles on specific brain tumor lesions.
