 Autoimmune polyendocrine syndrome, candidiasis, and ectodermal dystrophy (APEDED).
Autoimmune polyendocrine syndrome, candidiasis, and ectodermal dystrophy (APEDED).
APEDED type 1 is a subtype of autoimmune polyendocrine syndrome.
It is a life-threatening, multi organ or immune condition for which immunotherapy treatments have not been established.
It causes the dysfunction of multiple endocrine glands due to an autoimmune process.
It is a genetic disorder, inherited in autosomal recessive fashion.
It Is due to a defect in the AIRE gene (autoimmune regulator), which is located on chromosome 21.
The AIRE gene may be affected by any of at least 90 mutations.
Different mutations are seen in different geographic regions.
Mutations may be inherited in an autosomal recessive manner.
The AIRE gene confers immune tolerance.
AIRE is a transcriptional activator and enforces central T cell tolerance, mechanism for preventing auto immunity.
AIRE deficiency is characterized by excessive, multi organ interferon gamma, mediated responses.
APS-1 tends to cause severe symptoms present from early in life, usually around 3.5 years of age.
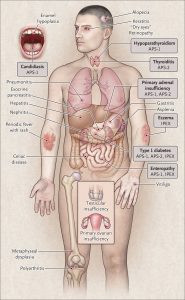
Common symptoms of APS-1 include:
Chronic mucocutaneous candidiasis.
Hypoparathyroidism.
Addison’s disease.
Ectodermal dystrophy of skin, dental enamel, and nails.
APS-1 may be associated with:
Autoimmune hepatitis.
Hypogonadism.
Vitiligo.
Alopecia.
Malabsorption.
Pernicious anemia.
Cataract.
Cerebellar ataxia.
APS-1 causes reactions with both interferon omega, interferon alpha. And interleukin 22, leading to damage to endocrine organs.
Common problems include hypercalcemis, nephrocalcinosis pituitary problems, and hypoparathyroidism.
Diagnosis of APS-1 is based on endoscopy, a CT scan, a biopsy and serum endocrine autoantibody screening.
Treatment
Autoimmune polyendocrine syndrome type 1 treatment is based on the symptoms.
The goals of medical management include screening for the development of new clinical manifestations, hormone replacement for endocrine disease and immunotherapies targeted to specific non-endocrine auto immune conditions, such as hepatitis, pneumonitis, and pancreatitis.
Treatments may involve hormone therapy, systemic antifungal treatments,and immunosuppression.
JAK inhibition with ruxolitinib shows promising results: decreases level of T cell derived interferon-gamma, normalized, Interferon-gamma, and CXCL9 levels, and caused remission of alopecia, oral candidiasis, nail dystrophy, gastritis, enteritis, arthritis, Sjogren-likesyndrome, urticaria, and thyroiditis.
