 Referred to as fertility treatment.
Referred to as fertility treatment.
Some forms of ART may be used with regard to fertile couples for genetic purpose.
Assisted conception accounts for 5% of US births.
ART may also be used in surrogacy arrangements.
With ART, sexual intercourse is bypassed and fertilization of the oocytes occurs in the laboratory environment.
ART procedures involve surgically removing eggs from a woman’s ovaries, combining them with sperm in the laboratory, and returning them to the woman’s body or donating them to another woman.
ART does not include treatments in which only sperm are handled, as with intrauterine—or artificial—insemination, or procedures in which a woman takes medicine only to stimulate egg production without the intention of having eggs retrieved.
Ovulation induction stimulates development of ovarian follicles by fertility medication to reverse anovulation or oligoovulation.
Ovulation induction medications are given by injection for 8 to 14 days: monitoring the development of the eggs using transvaginal ultrasound and blood tests to assess follicle growth and estrogen production by the ovaries. The endometrium permits embryo implantation only during the receptive phase, which falls 6 to 12 is after ovulation.
When follicles have reached an adequate size and the eggs are mature enough, an injection of the hormone hCG initiates the ovulation process.
Egg retrieval should occurs from 34 to 36 hours after the hCG injection.
In vitro fertilization is the technique of letting fertilization of the male and female gametes (sperm and egg) occur outside the female body.
Techniques for in vitro fertilization include:
Transvaginal ovum retrieval (OVR) is the process whereby a small needle is inserted through the back of the vagina and guided via ultrasound into the ovarian follicles to collect the fluid that contains the eggs.
Embryo transfer is the step in the process whereby one or several embryos are placed into the uterus of the female with the intent to establish a pregnancy.
Less commonly used techniques in in vitro fertilization are:
Assisted zona hatching (AZH) is performed shortly before the embryo is transferred to the uterus.
With assisted zona hatching a small opening is made in the outer layer surrounding the egg in order to help the embryo hatch out and aid in the implantation process of the growing embryo.
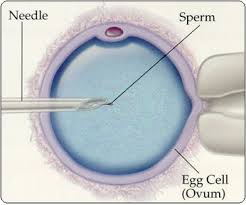
Intracytoplasmic sperm injection (ICSI) is used in the case of male factor infertility where sperm counts are very low or failed fertilization occurred with previous IVF attempts.
Intracytoplasmic sperm injection involves a single sperm carefully injected into the center of an egg using a microneedle: only one sperm per egg is needed.
When donor sperm is used, without ICSI, 50,000 and 100,000 sperm are used.
Autologous endometrial coculture is a possible treatment for patients who have failed previous IVF attempts or who have poor embryo quality.
Autologous endometrial coculture is achieved as the patient’s fertilized eggs are placed on top of a layer of cells from the patient’s own uterine lining, creating a more natural environment for embryo development.
Zygote intrafallopian transfer (ZIFT), is a process used where egg cells are removed from the woman’s ovaries and fertilized in the laboratory, and the resulting zygote is then placed into the fallopian tube.
Cytoplasmic transfer refers to the technique in which the contents of a fertile egg from a donor are injected into the infertile egg of the patient along with the sperm.
Egg donors are provided to women: with no eggs due to surgery, chemotherapy, or genetic causes; or with poor egg quality, previously unsuccessful IVF cycles or advanced maternal age: eggs are retrieved from a donor’s ovaries, fertilized in the laboratory with the sperm from the recipient’s partner, and the resulting healthy embryos are returned to the recipient’s uterus.
Sperm donation may provide sperm used in IVF procedures where the male partner produces no sperm or has an inheritable disease, or where the woman being treated has no male partner.
Preimplantation genetic diagnosis (PGD) involves the use of genetic screening mechanisms such as fluorescent in-situ hybridization (FISH) or comparative genomic hybridization (CGH) to identify genetically abnormal embryos.
PGD is an adjunct to ART procedures, and requires in vitro fertilization to obtain oocytes or embryos for evaluation.
Embryo splitting can be used for twinning to increase the number of available embryos.
Embryos are generally obtained through blastomere or blastocyst biopsy performed around day 5 or 6 of development.
Sex selection to achieve a desired sex in case of X chromosome linked diseases, can be accomplished in several ways, both pre- and post-implantation of an embryo, as well as at birth.
Other assisted reproduction techniques include:
Mitochondrial replacement therapy carry genes for mitochondrial diseases.
Gamete intrafallopian transfer (GIFT) a mixture of sperm and eggs is placed directly into a woman’s fallopian tubes using laparoscopy following a transvaginal ovum retrieval.
Reproductive surgery: fallopian tube obstruction and vas deferens obstruction, or reversing a vasectomy by a reverse vasectomy.
Surgical sperm retrieval (SSR) the reproductive urologist obtains sperm from the vas deferens, epididymis or directly from the testis in a short outpatient procedure.
Eggs, sperm and reproductive tissue can be cropreserved for later IVF.
Some studies have suggested that assisted reproductive technology is associated with an increased risk of birth defects.
Artificial reproductive technology could be an increased risk for medical complications with both the mother and baby: low birth weight, placental insufficiency, chromosomal disorders, preterm deliveries, gestational diabetes, and pre-eclampsia.
A US study showed 6.2% of IVF-conceived children had major defects, as compared with 4.4% of naturally conceived children matched for maternal age and other factors.
ART carries with it a risk for heterotopic pregnancy, which is asimultaneous intrauterine and extrauterine pregnancy.
The main risks of ART are
Genetic disorders
Low birth weight In IVF and ICSI,
Decreased expression of proteins in energy metabolism.
Children born after IVF are roughly twice as likely to have cerebral palsy.
Sperm donation has a birth defect rate of almost a fifth compared to the general population.
No significant differences are observed in the frequency or spectrum of mutations between naturally conceived fetuses and assisted-conception fetuses.
Little or no increased risk for postpartum depression among women who use ART.
Usage of assisted reproductive technology including ovarian stimulation and in vitro fertilization have been associated with an increased overall risk of childhood cancer in the offspring, which may be caused by the same original disease or condition that caused the infertility or subfertility in the mother or father.
Infants born after ART have similar neurodevelopment than infants born after natural conception.
Children born after fertility treatments have a higher risk of adverse perinatal outcomes, including prematurity, low birthweight, and congenital malformations.
The use of frozen embryo transfer is associated with small but statistically significant increase risk for childhood cancer.
