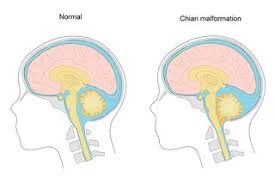
 A congenital herniation of the cerebellum through the foramen of magnum.
A congenital herniation of the cerebellum through the foramen of magnum.
Arnold–Chiari malformation, or Chiari malformation, is a malformation of the brain.
It consists of a downward displacement of the cerebellar tonsils through the foramen magnum, sometimes causing non-communicating hydrocephalus as a result of obstruction of cerebrospinal fluid outflow.
Obstruction of cerebrospinal fluid outflow can cause headaches, fatigue, muscle weakness, difficulty swallowing, dizziness, nausea, impaired coordination, and, in severe cases, paralysis.
Nystagmus is often very commonly present with Chiari malformation.
Occurs in 1 in 1000 live births.
Divided into IV types of malformation.
Type I is a congenital malformation that is generally asymptomatic during childhood, but often manifests with headaches and cerebellar symptoms of imbalanced gait and neck pain.
Type I: herniation of cerebeller tonsils, only.
Herniation of cerebellar tonsils, tonsillar ectopia of more than 3 mm below foramen magnum, syringomyelia of cervical or cervicothoracic spinal cord can be seen.
The syndrome of occipitoatlantoaxial hypermobility can be an acquired Chiari I malformation in patients with hereditary disorders of connective tissue such as Ehlers-Danlos syndrome or Marfan Syndrome.
Type II usually accompanied by a lumbar myelomeningocele or lumbosacral spine with tonsillar herniation below the foramen magnum, which is less pronounced than that seen with Chiari I.
Type II malformation is associated with a larger cerebellar vermian displacement.
Chiarii II Malformation includes herniation of the cerebellum vermis and medulla into the spinal canal, which obstruct the flow of CSF around the lower brainstem causing ventricular dilatation and increased intracranial pressure and cystic dilatation of the spinal cord, syringomyelia.
Type II: associated with breaking of the tectal plate, aqueductal stenosis, herniation and unrolling of the vermis into the vertebral canal, stretching of the cranial nerves IX, X, and XI.
Type II malformation anatomic findings include a low lying torcular herophili, tectal beaking, and hydrocephalus with consequent clival hypoplasia.
Type III malformation is associated with an occipital encephaloceles containing a variety of abnormal neuroectodermal tissues.
Type II malformation associated with syringomyelia and hydrocephalus.
Type IV malformation is characterized by a lack of cerebellar development in which the cerebellum and brain stem lie within the posterior fossa with no relation to the foramen magnum.
Type IV malformation is associated with hypoplasia and is not compatible with life.
Some processes associated with Chiari Malformation include hydrocephalus, syringomyelia, spinal curvature, tethered spinal cord syndrome, and connective tissue disorders such as Ehlers-Danlos syndrome and Marfan Syndrome.
Chiari Type 1 malformations occur occur by a reduction or lack of development of the posterior fossa as a result of either congenital or acquired disorders.
Chiarri 1 malformation can be associated with a non-communicating hydrocephalus or cervicothoracic syringomyelia.
Congenital causes include hydrocephalus, craniosynostosis, hyperostosis, X-linked vitamin D-resistant rickets, and neurofibromatosis type I.
Acquired disorders of Chiari Type 1 malformations include space occupying lesions such as brain tumors or hematomas.
The prevalence of Chiari I malformation is estimated to be in the range of one per 1000 to one per 5000 individuals.
Diagnosis is made by patient history, neurological examination, and Magnetic Resonance Imaging, the best imaging modality.
Computed tomorgraphy (CT) can miss spinal cord cavitations.
Neuroradiological imaging is required to rule out any other intracranial condition that could account for intracranial pressure and tonsillar herniation.
Imaging evaluates the neural structures within the posterior cranial fossa and their impact on the foramen magnum.
Multiplanar CT is the best diagnostic approach for imaging of syringomyelia and prolapse of the vertebral column into the cranial cavity.
The diagnosis of a Chiari II Malformation can be made prenatally by ultrasound exam.
Treatment for Chiari malformation are based on clinical symptoms rather than the radiological findings.
The presence of a syrinx causes specific signs and symptoms from dysesthetic sensations to spasticity and paresis, and may require decompressive surgery.
Chiari Malformation Type II requires immediate surgery due to severe brain stem damage and neurological impairment.
Decompressive surgery to reduce pressure usually removes the lamina of the first, second or even third cervical vertebrae and part of the occipital bone of the skull.
Detethering the spinal cord is an alternate approach to relieve the compression of the brain against the foramen magnum, obviating the need for decompression surgery.
Complications of decompression include bleeding, damage to structures in the brain and spinal canal, meningitis, CSF leaks, occipito-cervical instability and pseudomeningeocele.
Type II lesions may also present with syringomyelia in C8-T1 and lumbar meningomyelocele.
