
Most common valvular disease.
Risk factors include the presence of a bicuspid aortic valve, present in one to 2% of the population worldwide, and aortic sclerosis defined as focal areas of leaflet thickening and mild calcification.
AS effects approximately 25% people older than 65 years, with approximately a 2% an annual rate of progression to clinical AS.
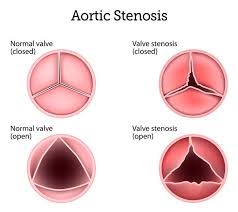
Aortic stenosis is defined as a valve leaflet disease with left ventricle outflow obstruction and is most commonly caused by calcification of a congenital bicuspid or normal trileaflet valve, although aortic stenosis due to rheumatic heart disease occurs in areas of the world where rheumatic fever is endemic.
The most common predisposition to AS is congenital bicuspid aortic valve accounting for up to 50% of all aortic valve interventions.
Nearly all patients with congenital bicuspid aortic valve, eventually require valve intervention, although often not until age 60 to 80 years.
In patients undergoing aortic valve replacement for severe AS, congenital bicuspid severe valve disease accounts for more than 80% of patients younger than 60 years and approximately 50% of those older than 60 years.
The pathophysiology of AS has been attributed to mechanical trauma of repeated aortic valve closure, but presently evidence suggest it begins as an inflammatory process involving biochemical, humoral and genetic factors: similar to atherosclerosis, including accumulation of low density lipo protein and lipoprotein (a), macrophage and lymphocyte infiltration, activation of inflammatory pathways, and tissue calcification.
Most prevalent form of heart valve disease in the developed world.
AS is a slowly progressive, chronic disease in patients are asymptomatic until the aortic valve obstruction is sufficiently severe to limit the normal in increase in cardiac output that occurs with exercise.
Population-based prevalence of moderate or severe AS in the US estimated to be as high as 4.6%.
Calcific AS affects approximately 12.6 million people globally and more than 100,000 deaths annually.
Prevalence of AS is higher in high income countries compared with low and middle income countries.
In the US AS affects one to 2% of patients age 65 or older and 12% of those older than 75 years.
AS has a cumulative incidence of clinically significant AS of 2.8 to 3.7% in longitudinal population based follow up studies.
In 2021 more than 40,000 surgical aortic valve replacements and 80,000 trans catheter aortic valve implantations were performed in the US.
Results in progressive disease that results in stiff valve leaflets with eventual obstruction to left ventricular outflow.
The normal aortic valve consists of three, pliable, leaflets that allow ejection to blood from the heart during systole and prevent backflow of blood during distole.
AS is the result of the leaflets becoming thickened, fibrosed, and calcified leading to rigid leaflets with high resistance to valve motion and obstruction of the antegrade blood flow.
Presents as a mechanical obstruction to ventricular ejection at the aortic valve level, worsens overtime, and with the onset of symptoms there is a rapid decline that results in progressive part failure and death.
Diagnosis of AS is challenging due to symptoms of exercise intolerance, dyspnea on exertion and dizziness occur late in disease, and may be caused by other cardiac conditions or pulmonary conditions.
Physical examination is not reliable for detection of AS or evaluation of its severity.
Findings of a loud, late peaking systolic murmur radiating to the carotid artery, a single quiet second heart sound, and a delayed diminished carotid, upstroke are findings of AS, but occur with ;severe disease, making them relatively insensitive for diagnosis earlier in the course.
Symptomatic severe aortic stenosis has a two-year mortality rate of nearly 50%.
The aortic leaflets undergo progressive calcification and fibrosis, resulting in narrowing of the valve and the development aortic stenosis.
Persistent pathologic stimuli result in accumulation of fibrotic collagen and the development of calcific nodules, which compromise the biomechanical integrity of the cusps of the aortic valve and lead to stenosis.
Endothelial to mesenchymal transition occurs with pathologic aortic valve remodeling.
Family analysis suggests a strong genetic contribution to the risk of aortic stenosis, and persons with at least one sibling who had aortic stenosis have been found to be at significantly higher risk for the development of aortic valve disease than those who do not: the risk increases further when two or more siblings have aortic stenosis.
A progressive disease process in which the end stage is associated with obstruction of the left ventricle outflow, resulting inadequate cardiac output, decreased exercise capacity, heart failure, and death from cardiovascular causes.
Stage A occurs when risk factors are present, but vave function is normal
Stage B occurs when there is mild to moderate AS with the velocity of 2.0 to 3.9 ms, in patientS with stage B left ventricular systolic function is typically normal, although diastolic dysfunction may be present.
Stage C includes asymptomatic patients with severe valve obstruction with aortic velocity 4 ms of higher or mean gradient 40 mm Hg mercury or higher Typically the valve is less than equal to 1 cm².
Stage D is defined as symptomatic severe AS.
AS increases pressure in the left ventricle leading to myocardial hypertrophy, diastolic dysfunction, and eventually heart failure.
AS causes symptoms by inadequate increase in cardiac output during exercise, which may lead to ischemia, decreased blood pressure, impaired LV function and increased diastolic filling pressure which may cause dyspnea due to pulmonary congestion.
Measures to prevent or reverse AS are lacking.
Chronic pressure overload due to aortic stenosis promotes left ventricular remodeling by muscle fiber hypertrophy and abnormalities of the collagen network, and resulting diastolic dysfunction and increased risk of heart failure.
Myocardial fibrosis persists after aortic valve replacement and reduction of myocardial hypertrophy, resulting in persistent diastolic stiffness.
Classical symptoms of hemodynamically significant AS include heart failure, syncope, and angina and symptoms manifest once the valve narrowing has become severe and indicate a poor prognosis unless intervention is performed.
Symptom triad of angina, syncope, and dyspnea represents a late consequence of
Chronic progressive left ventricular overload caused by worsening aortic stenosis which has developed over several decades.
Natural history is of protracted symptom-free latent period, with increasing obstruction and myocardial overload followed by abrupt onset of severe symptoms of angina, syncope, and dyspnea, with nearly uniform mortality within five years of onset.
Obstruction at the level of the aortic valve causes increased pressure within the heart’s left ventricle.
Obstruction of the aortic valve can lead to hypertrophy and ultimately dysfunction of the heart.
While x-ray and ECG might indicate aortic stenosis, echocardiography is the diagnostic procedure of choice.
The most common intervention is surgical aortic valve replacement with a bioprosthetic or mechanical valve.
Aortic valve replacement accounts for at least 16% of all cardiac surgeries and the majority of all trans catheter valve procedures.
Indications for trans catheter aortic valve replacement have been expanding and is used especially in patients with excessive surgical risk.
Aortic valve replacement by surgical or transcatheter approach remains the cornerstone of treatment, and is reserved for patients with severe aortic stenosis who are symptomatic or those with the left ventricular ejection fraction below 50%.
Guidelines recommend prompt surgical aortic valve replacement or trans aortic valve implantation.
PARTNER trial demonstrated high early mortality of untreated disease which showed 50% mortality at one year and more than 90% of five years demonstrating need for accurate and early diagnosis.
There is a high mortality rate associated with severe symptoms, which is about 50% at one year with standard medical care.
Studies suggested severe AS is untreated in the US with only about 48% undergoing surgical or trans aortic valve replacement.
Presently asymptomatic patients with severe AS do not receive aortic valve replacement routinely.
Aortic valve replacement is not recommended for patient with moderate AS.
Prevalence increases from 0.2% in adults 50-59 years of age to 2.8% in adults older than 75, to9.8% in octogenarians.
Prevalence 0.4%.
Three of 100 individuals between the ages of 75-85 years have this lesion.
Calcific degenerative aortic stenosis is the most common valve disease because of aging population.
Aortic valve calcification is felt to be an active, multifactorial disease process, with osteogenic pathways participating in its development.
Characteristic heart murmur which is typically holosystolic and has a crescendo-decrescendo, diamond shaped character.
Systolic murmur is usually loudest at the base and radiates into the neck.
Rheumatic aortic stenosis leads to leaflet thickening and fusion to a narrow oval residual orifice.
With degenerative calcific aortic stenosis patients are typically greater than 70 years of age, and their residual orifice retains a Y or branch opening configuration.
Key factor leading to the development of calcific aortic stenosis secondary to mechanical stress.
Degenerative calcific AS is a consequence of aging and is a result of a biologically active process with features of an osteoblast phenotype.
Affect about 3% of elderly and is the most common reason for valve replacement.
Prevalence increases with increasing average lifespan and echocardiographic studies estimate that there is moderate or severe disease in 5% of patients older than 75 years in the US.
Approximately 65,000 aortic valve replacements performed in the US in 2010.
Aortic valve replacements are done primarily for aortic stenosis, and 70% of these procedures are performed in patients older than 65 years of age.
Prevalence of aortic valve sclerosis is approximately 26% and in patients over the age of 65 years it is 37%.
About 10-20% of patients with aortic sclerosis will progress to hemodynamically significant aortic stenosis over 10-15 years.
Risk factors for progressive disease mirror those of coronary artery disease.
No medical therapies are available presently that slow progression of aortic stenosis.
Risk factors include advanced age, male sex, bicuspid valves, hypertension, hyperlipidemia, diabetes, smoking, and renal dysfunction.
Cholesterol lowering and anti-inflammatory agents do not slow the disease process, as with coronary artery disease.
May have an inflammatory basis with increased markers of macrophage activity.
Subgroups of families have bicuspid valves that are inherited in an autonomic dominant pattern.
A dilated ascending aorta may accompany biscuspid valves, and a number of patients with congenital aortic stenosis have coarctation of the aorta.
Mutations of the signaling and transcriptional regulator gene NOTCHI has been identified in families with biscuspid aortic valves and leaflet calcification.
Factors associated include older age, male gender, elevated levels of low density lipoprotein and lipoprotein(a), smoking abuse, hypertension, diabetes and the metabolic syndrome.
Hypertension affects 30 to 79% of patients with AS, and this associated with increased valve calcification.
Genetic variation in the LPA locus mediated by lipoprotein (a) levels is associated with aortic valve calcifications among multiple ethnic groups with critical aortic stenosis (Thanassouls G et al).
May coexist with hypertrophic obstructive cardiomyopathy.
Patients with AS are at increased risk of developing infective endocarditis:greater than eight times higher than in the general population.
BNP of greater than 550npg/mL associated with poor prognosis.
Helpful testing includes: exercise tests to ascertain symptoms or high-risk features, cardiac CT scans to quantify severity and progression of aortic valve calcifications, and serial measurements of BNP as a biomarker of disease severity and progression.
Gradually progressive disease with a long asymptomatic phase, lasting decades, followed by a shorter symptomatic phase.
Aortic stenosis associated with gout, and patients with gout are more likely to develop severe aortic disease.
To maintain cardiac output compensatory changes occur including increases in the left ventricular wall thickness and contractility.
When compensatory changes are overwhelmed diastolic compliance decreases, subendocardial ischemia occurs, exhausted myocardial contractile reserve followed by irreversible myocardial fibrosis and baro receptor activated vasodilation.
The above changes lead to reductions in cardiac output and pulmonary congestion.
Sudden cardiac death is not common in aortic stenosis but it may result from multi-factorial factors of low cardiac output, ischemia and arrhythmias.
Approximately half of all untreated patients die in the first two years after symptoms appear.
Mortality is not increased in asymptomatic patients.
Rate of death is more than 50% at two years for patients with symptomatic disease unless aortic valve replacement is performed.
Onset of symptoms is associated with poor prognosis.
Leading cause for valve replacement in the U.S.
No known therapy exists to prevent disease progression.
Most cases are the result of bicuspid aortic valves or calcific involvement of a tricuspid aortic valve.
Patients with bicuspid aortic stenosis may present in their 50s, whereas those with the senile calcific aortic stenosis can present as late as their 80s.
Congenitally bicuspid valve, present in 0.5-0.8% of the population the underlying anatomy in the majority of valve replacements for aortic stenosis.
Usually diagnosed incidentally by cardiac auscultation or by echocardiographic studies for other indications.
The number of cases from rheumatic disease has dwindled.
Lesions characterized by subendothelial thickening, basement membrane disruption, accumulation of lipids, cellular infiltration along with fibrosal thickening with lipids, protein, and calcium accumulation.
Severity ranges from mild leaflet thickening without valve obstruction, i.e., aortic sclerosis to severe aortic stenosis.
Abnormalities of the valves lead to thickened and stiff valvular cusps with little systolic excursion and obstruction of the left ventricular outflow.
Survival of patients with aortic stenosis is nearly normal until the onset of symptoms, when survival rates decrease sharply.
Most patients who develop symptoms are older than 80 years of age.
Patients with severe AS who develop angina, dyspnea, lightheadedness, or syncope have a class I indication for aortic valve replacement.
Exercise testing can uncover symptoms in seemingly asymptomatic patients.
The main feature in severe aortic stenosis is the presence of calcification in the valve.
After the onset of symptoms the average survival is only two-three years.
Transthoracic echocardiogram is recommended as the initial evaluation of patients with known or suspected AS to confirm the diagnosis and determine the need for treatment.
Electrocardiography is the primary diagnostic test and should be done to assess valve anatomy, hemodynamics, concomitant lesions and left ventricular function.
Classification of aortic stenosis severity
U/S findings Mild Moderate Severe
Aortic valve area, cm2 >1.5 1.0-1.5 <1.0
Aortic valve area index, cm2/m2 – – 0.6
Mean pressure gradient, mmHg 25 25-40 >40
Peak jet velocity, m/s <3 3-4 >4
Peak aortic valve velocity greater than 4 m/s identifies most patients with hemodynamically severe AS.
Severe aortic stenosis is defined as the mean gradient greater than 40 mmHg, peak aortic jet velocity greater than 4,m/s and aortic valve area smaller than 1 cm² or velocity greater than 4 milliseconds.
Normal aortic valve velocity of one millisecond increasing progressively as valve narrowing worsens from mild with a velocity of 2 to 2.9 ms to moderate velocity of 3 to 3.9 ms and severe valve obstruction velocity upgraded in 4 ms.
Aortic valve replacement is indicated for patients with severe aortic stenosis with aortic valve area less than 1 cm², who have symptoms, have left ventricle dysfunction, or undergoing cardiac surgery for another indication.
In a trial of patients with asymptomatic but very severe aortic stenosis randomized to surgical valve replacement or conservative follow up care: at 30 days after surgery death for any cause, hospitalization for heart failure were significantly better among patients who were doing surgical valve replacement promptly rather than those assigned to conservative care (Kang D).
Nearly 30% of patients with severe symptomatic aortic stenosis are not candidates for surgical aortic valve replacement because of multiple medical comorbidities, advanced age, prior surgery, or high risk anatomic features.
Approximately 20% of patients with severe AS present with low left ventricular stroke volume and low gradients.
The administration of an inotropic agent such as dobuamine, augments cardiac output and allows a more accurate assessment of the severity of AS.
Aortic stenosis severity can be determined from aortic valve area in patients with reduce stroke volume.
Approximately 75% of patients with aortic stenosis will be dead three years after the onset of symptoms if the aortic valve is not replaced.
At least 30% of patients with severe symptoms do not undergo surgery because of advanced age, left ventricular dysfunction, or comorbidities.
A valve area of less than 0.8 cm2 or a gradient of more than 50 mm Hg represents critical stenosis capable of causing symptoms or death.
A transvalvular gradient of 50 mm HG or greater has a positive predictive for severe stenosis of 90% , but a gradient of less than 50 mm Hg is compatible with mild, moderate or severe aortic stenosis.
Early lesions are located on the aortic side of the valve in regions with low shear stress.
Poor outcome with congestive heart failure, angina and syncope.
Patients with severe aortic stenosis should undergo echocardiography annually.
In patients with mild to moderate aortic stenosis performance of echocardiography should be done every two to five years.
CT imaging of the chest can quantify, leaflet calcification, and define AS severity and can be helpful to define specific anatomic factors such as annulus size, coronary Ostia position, and vascular access, which affect the feasibility of a transcatheter approach.
Presently there is no medical therapy and only aortic valve replacement will relieve mechanical obstruction.
1-2% of live births are associated with bicuspid aortic valves.
Symptomatic aortic stenosis secondary to bicuspid valve usually seen from the late 40’s to late 60’s.
Atherosclerosis of the tricuspid valve is seen in patients older than 70 years.
Acquired 2A von Willebrand syndrome occurs commonly in patients with severe aortic stenosis.
Heyde’s syndrome is a form of type IIA Von Willebrand’s syndrome, angiodysplastic bleeding and aortic calcification stenosis.
Associated with typical systolic ejection murmur.
Systolic ejection click may precede the murmur in cases of mild-moderate to stenosis when the valve is still pliable.
Classic aortic murmur heard at the aortic area and transmitted to the neck and apex of the heart,
Severe AS associated with heave, weak or bsent aortic second sound, or reversed splitting of th second sound.
When aortic valve area is less than 0.8-1cm2 the ventricular systole is prolonged, carotid pulsation is associated with a delayed upstroke and low amplititude.
With increasing stenosis LVH occurs with increased ventricular end-diastolic pressure.
With severe valve stenosis heart failure, angina or syncope may occur as presenting symptoms, and may all be precipitated by exertion.
Heart failure may occur suddenly or gradually.
Impaired perfusion of the endocardium may result in angina.
50% of patients with calcified aortic stenosis have associated coronary artery disease.
Syncope may be seen with exertion as increased LV pressures cause LV baroreceptors to precipitate peripheral vasodilation.
Syncope may also be seen in AS due to calcific invasion of the conducting system leading to arrhythmias.
Patients with bicuspid valvular disease require surgery a decade earlier than those with tricuspid stenosis.
An association suggested between calcific aortic stenosis and genetic polymorphisms in vitamin D receptor, estrogen receptor, apolipoprotein E4, and interleukin10 alleles.
Calcified aortic stenosis associated with elevated serum lipids, accumulation of lipid in aortic leaflets and increased risk of atherosclerosis.
In a randomized clinical trial of aggressive lipid lowering does not affect hemodynamic progress or the time to valve replacement in adults with aortic stenosis (Rossebo).
Progression of aortic stenosis parallels aortic valve sclerosis which shares similarities to the process of atherosclerosis.
Control of lipoprotein abnormalities can slow the development of aortic sclerosis.
EKG reveals LVH in most patients, but can be normal in 10% of patients.
Chest X-ray usually shows a normal or enlarged heart silhoutte,calcified aortic valve, calcification of the aorta and aortic dilation.
Echocardiogram provides information about aortic valve calcifications, LV thickness, LV function and estimate of aortic valve gradient.
Heart catheterization provides hemodynamic information and coronary artery evaluation.
Valve gradients can be measured at catheterization, and estimates valve area.
Doppler can derive peak gradient results.
In the presence of heart failure, angina or syncope 50% 3 year mortality without surgery.
Aortic valve replacement is definitive therapy for severe symptomatic stenosis.
Surgery indicated in all symptomatic patients with significant AS.
Valve replacement not indicated in asymptomatic individuals, unless peak gradient exceeds 64 mm Hg or a mean Doppler gradient exceeds 40 mm Hg.
Associated with high rate of death when sympyomatic, if left untreated.
Patients with advanced age, poor left ventricular function have increased operative complications or death.
Mortality of aortic valve replacement 2-5%.
Operative mortality increases with number and severity of coexisting illnesses.
Mortality rates for aortic valve replacement is higher in patients with associated ischemic cardiomyopathy.
Coronary artery bypass for coronary artery disease is usually done at the same time of aortic valve replacement.
Percutaneous valvuloplasty may be helpful in the young and adolescent patients, but is subject to early stenosis in the elderly and is used rarely used in this group.
Aortic balloon valvuloplasty is only beneficial in patients with preserved LV function, a group that comprises excellent candidates for aortic valve replacement.
Transcatheter aortic valve replacement replaces the native valve with a bioprosthetic valve delivered on a catheter through the femoral artery or left ventricular apex.
Approaches may be transarterial, or transapical.
In a study of 3195 highly symptomatic patients at high risk undergoing transcatheter aortic valve implantation had a 30 day and 1 year death rate of 9.7% and 24%, respectively, 1 year stroke incidence of 4.1% and periprosthetic aortic regurgitation64.5% (Glard M et al).
Among patients with aortic stenosis at intermediate surgical risk there is no significance in the incidence of death or disabling stroke at five years after transcatheter aortic valve replacement as compared with surgical aortic valve replacement (MakkarRR).
More than 50,000 patients have been treated with transcatheter aortic valve implantation.
Transcatheter aortic valve implantation removes calcified cusps and forcibly spread stenotic aortic valve cusps and anchor stented bio prostheses without sutures.
A subgroup of patients with AS not candidates for surgical aortic valve replacement who underwent transfemoral aortic valve replacement had a improvement of 20% in 1 yar survival rate and reduced symptoms (Leon MB et al).
In a randomized study of 699 high risk patients with severe AS underwent either transcatheter aortic valve replacement with a balloon expandable bovine pericardial valve or surgical relpacement: similar rates of survival at 1 year (Smith CR et al).
In the above study death rates were 3.4% in the transcatheter group and 6.5% in the surgical group at 30 days, 24.2% and 26.8%, respectively , at 1 year.
Among patients age 70 years older with severe, symptomatic aortic stenosis and moderately increase operative risk, trans aortic valve implantation was is non-interior to surgery with respect to all cause mortality at one year (UK TAVI Trial Investigators): mortality at one year was 4.6 percent with TAVI versus 6.6% with surgery.
Guidelines, recommend transfemoral aortic valve implantation for patients with symptomatic AS who are unable to undergo surgery or have a high estimated surgical mortality risk of greater than 8%.
Guidelines recommend surgical aortic valve replacement for adults younger than 65 years, with a mechanical valve preferred over a bioprosthetic valve in those younger than 50 years based on expected years of remaining life and valve durability.
TAVI is recommended for individuals age 75-80 years and older.
In asymptomatic patients with severe aortic stenosis and myocardial fibrosis, early aortic valve intervention had no demonstrable effect on all cause death or AS related hospitalizations (EVOLED investigators).
Among older adults with AS undergoing TAVI who were at high risk for heart failure events SGLT2 inhibitors resulted in significantly lower incidence of death for many cause of worsening heart failure than standard care alone.
In younger patients the Ross procedure is a viable option of replacing the aortic valve with the patient’s pulmonary valve and then replacing the latter valve with a homograft.
Surgery is the only treatment documented to reduce mortality.
Aortic valve replacement decreases mortality, relieves symptoms due to AS, results in a regression of left ventricular hypertrophy, and improves left ventricular systolic function.
Aortic valve replacement with a prosthetic valve requires long-term management, including lifelong antithrombotic therapy with a mechanical aortic valve, endocarditis prevention, and valve monitoring for deterioration and dysfunction.
Following surgical aortic valve replacement with a bioprosthetic valve freedom from valve deterioration at 10 years is 94%, 81.7% at 15 years and 52% of 20 years.
The valve durability of bioprosthetic TAVI valves is similar to surgical implanted valves in older adults with duration of follow up of 5 to 10 years.
Mortality and mobility rates are twice the risk of original surgery when repeat valve surgery is necessary.
Prosthetic valve endocarditis occurs at a rate of .3 to 1.2% per patient year, and is associated with a mortality rate of 20% or higher compared to 5% or lower in patients with native valve endocarditis.
Guidelines recommended antibiotic prophylaxis program for all patients with a prosthetic valve undergoing dental procedures, including routine cleanings.
