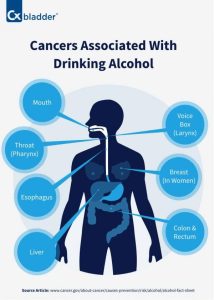
 Alcohol causes cancers of the oesophagus, liver, breast, colon, oral cavity, rectum, pharynx and laryngeal cancers, and probably causes cancers of the pancreas.
Alcohol causes cancers of the oesophagus, liver, breast, colon, oral cavity, rectum, pharynx and laryngeal cancers, and probably causes cancers of the pancreas.
Consumption of alcohol in any quantity can cause cancer, but the more alcohol is consumed, the higher the cancer risk,
and no amount can be considered safe.
Alcoholic beverages are classified as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC).
3.6% of all cancer cases and 3.5% of cancer deaths worldwide are attributable to consumption of alcohol.
Aetaldehyde, a metabolic derivative of ethanol causes cancer.
740,000 cases of cancer in 2020 or 4.1% of new cancer cases were attributed to alcohol.
Alcohol is thought to cause cancer through three main mechanisms:
DNA methylation
Oxidative stress
Hormonal alteration
Secondary mechanisms of cancer formation include: liver cirrhosis, microbiome dysbiosis, reduced immune system function, retinoid metabolism, increased levels of inflammation, 1-carbon metabolism and disruption of folate absorption
Heavy drinking consisting of 15 or more drinks per week for men or 8 or more drinks per week for women beverages/week contributed the most to cancer incidence compared with moderate drinking.
The rate of alcohol related cases is 3:1 male:female, especially in o esophageal and liver cancers.
In 2020, approximately 740,000 cases of alcohol-related cancers were identified globally with 58% of cases (430,000) residing in Asia 25% of cases (180,000) residing in Europe 8% of cases (60,000) residing in North America, 5% of cases (39,000) residing in Latin America and the Caribbean, 3% of cases (23,000) residing in Africa
1% of cases residing in regions termed other.
More than three-quarters of the 740,000 cases were in men.
Approximately 4% of cancer-related deaths in the United States are attributed to alcohol consumption each year, with breast cancer and esophageal cancer deaths being the most common in women and men respectively.
An estimated 3.2% of cancer deaths in United States were attributed to alcohol consumption.
The International Agency for Research on Cancer of the World Health Organization has classified alcohol as a Group 1 carcinogen, similar to arsenic, benzene, and asbestos.
Alcohol increases the risk of developing breast cancer, liver cancer, colorectal cancer, esophageal cancers, pharyngeal cancer, laryngeal cancer, and oral cancer.
Acetaldehyde which is a metabolite of ethanol is also carcinogenic to humans.
Acetaldehyde is a byproduct of ethanol breakdown in the liver, metabolized by Alcohol dehydrogenase (ADH), Cytochrome P-450 and bacterial catalases.
The liver then normally eliminates 99% of the acetaldehyde.
ALDH2 converts Acetaldehyde into acetate which is a byproduct that can be excreted through the liver.
Those with ADH1B*1 have higher rates of conversion of ethanol into Acetaldehyde while, people with ALDH2*2 have a slower conversion rate of acetaldehyde to acetate causing faster build up of acetaldehyde concentrations.
28-45% of east asian populations carry the ALDH2*2 allele.
An average liver can process 7 grams of ethanol per hour.
It takes 12 hours to eliminate the ethanol in a bottle of wine, giving 12 hours or more of acetaldehyde exposure.
DNA Methylation is the addition of a methyl group to the carbon-5 of nucleotides.
The most common methylation site is onto a cystine preceding guanine nucleotides.
This methylation is catalyzed by DNA methyltransferase enzymes taking a methyl group from SAMe(S-Adenosyl-L-Methionine).
Heavy alcohol consumption is thought to cause epigenetic changes by decreasing the availability of SAMe thereby changing the methylation pattern of DNA causing hypo or hypermethylation resulting in alteration of DNA transcription.
Oxidative stress and ROS accumulation is a major player in cancer growth.
The metabolism of ethanol by CYP450 2E1 into acetaldehyde is a byproduct of ROS.
The presence of ROS in the cellular environment causes lipid peroxidation which can lead to exocyclic adducts.
ROS in a tumor microenvironment can also act as an intercellular signal leading to up-regulation of vascular endothelial growth factors and monocyte chemotactic protein-1.
The accumulation of iron is also found to correlate to alcohol consumption which leads to higher levels of peroxidation and resulting oxidative damage.
High levels of hormones in serum have been associated with heavy alcohol use: estrogen and estradiol can increase transcriptional activity in estrogen receptor positive cells which promote breast cell proliferation.
After menopause those with heavy alcohol consumption have higher risk for breast cancer and estrogen dependent cancers.
Heavy alcohol consumption can cause a decrease in folic acid availability which can decrease the availability of nucleotides for DNA repair.
Ethanol can decrease the conversion of homocysteine to methionine which is an essential amino acid that is part of the formation of SAMe.
Increased inflammation due to alcohol consumption can increase various cytokine formations especially NF-κB which is a transcription factor.
Alcohol usage is associated with lower Vitamin A levels which causes a reduction in retinoid conversion and signaling.
Individuals who both smoke and drink are at a much higher risk of developing mouth, tracheal, and esophageal cancer.
Ethanol is thought to potentially be a solvent for carcinogenic factors in smoking.
The risk of developing mouth, tracheal and esophageal cancers is 35 times higher than in individuals who neither smoke nor drink, suggesting a cocarcinogenic interaction between alcohol and tobacco-related carcinogens.
The risk of cancer associated with alcohol consumption is higher in tissues in closest contact on ingestion of alcohol, such as the oral cavity, pharynx and esophagus, as ethanol is a proven carcinogen.
Th metabolite of ethanol acetaldehyde that produced in the liver is highly carcinogenic, thus explaining both local (mouth, throat, esophageal cancers) as well as distant (skin, liver, breast) cancers.
Cytotoxic effect of ethanol on the cells lining the oral cavity, pharynx and esophagus are due to the activation of the division of the stem cells located in deeper layers of the mucosa to replace the dead cells.
Each time stem cells divide, they become exposed to errors associated with cell division-mutations arising during DNA replication and chromosomal alterations occurring during mitosis, and also become highly vulnerable to the genotoxic activity of DNA-damaging agents of acetaldehyde and tobacco carcinogens.
Alcohol consumption probably increases the risk of developing cancer of the oral cavity, pharynx and esophagus by promoting the accumulation of cell divisions in the stem cells that maintain these tissues in homeostasis.
The cytotoxic activity of ethanol is concentration-dependent, the risk of these cancers increase with increasing amounts of ethanol.
There is a synergistic effect of alcohol and tobacco use on the risk of cancers.
Alcohol stimulates the epithelial-mesenchymal transition (EMT), in which ordinary cancer cells change into a more aggressive form and begin to spread throughout the body.
Alcohol influences tumor volume doubling time in hepatocellular cancer.
Mutations in the enzymes involved in the production of acetaldehyde can lead to increased cancer risk: Cytochrome P450 2E1 and alcohol dehydrogenase.
Alcohol a known porphyrinogenic chemical has been linked the inherited hepatic porphyrias with a predisposition to hepatocellular carcinoma.
Tyrosinemia Type I, an inherited disorder in tyrosine metabolism impacting the second enzyme in the heme metabolic pathway is associated with a high risk of developing HCC in younger populations, including children.
Increasing but moderate alcohol consumption in women was determined to be associated with an increased risk of cancers of the oral cavity and pharynx, esophagus, larynx, rectum, breast, and live.
Alcohol consumption at any quantity is a risk factor for cancers of the mouth, esophagus, pharynx and larynx.
Risks increases above baseline with any alcohol intake (mild; <2 glass of wine per week) and increases significantly with moderate alcohol intake (one glass of wine per day) with highest risk in those with greater than 7 glasses of wine per week.
A drink is defined as 12 ounces of regular beer, 5 ounces of wine, or 1.5 ounces of 80-proof liquor.
Moderate alcohol drinking i up to one drink per day for women and up to two drinks per day for men.
Heavy alcohol drinking is defined as having more than three drinks on any day or more than seven drinks per week for women and more than four drinks on any day or more than 14 drinks per week for men.
A study in an Italian population characterized by frequent wine consumption, found wine the beverage most strongly related to the risk of laryngeal cancer.
A review of the epidemiological literature published from 1966 to 2006 concluded that:
The risk of esophageal cancer decreases rapidly and significantly after long periods of abstention.
Risk of head and neck cancer only reduced significantly after 10 years of cessation.
After more than 20 years of alcohol cessation, the risks for both cancers were similar to those seen in people who never drank alcohol.
For every additional drink regularly consumed per day, the incidence of oral cavity and pharynx cancers increases by 1 per 1000.
The incidence of cancers of the esophagus and larynx increase by 0.7 per 1000.
Acetaldehyde (a breakdown product of alcohol) is implicated in oral cancer.
Alcohol is a risk factor for breast cancer in women.
A woman drinking an average of two units of alcohol per day has an 8% higher risk of developing breast cancer than a woman who drinks an average of one unit of alcohol per day.
For every additional drink regularly consumed per day, the incidence of breast cancer increases by 11 per 1000.
Approximately 6% (between 3.2% and 8.8%) of breast cancers reported in the UK each year could be prevented if drinking was reduced to a very low level of less than 1 unit/week.
Moderate to heavy consumption of alcoholic beverages (at least three to four drinks per week) is associated with a 1.3-fold increased risk of the recurrence of breast cancer.
Further, consumption of alcohol at any quantity is associated with significantly increased risk of relapse in breast cancer survivors.
Drinking may be a cause of earlier onset of colorectal cancer.
The evidence that alcohol is a cause of bowel cancer is convincing in men and probable in women.
Alcohol is a risk factor for liver cancer, through cirrhosis.
Approximately 5 percent of people with cirrhosis develop liver cancer.
Cirrhosis is a disease that develops when liver cells are replaced with scar tissue after damage from alcohol abuse.
The chances of getting liver cancer increase markedly with five or more drinks per day.
It is estimated that for every additional drink regularly consumed per day, the incidence of liver cancer increases by 0.7 per 1000.
In the United States, liver cancer is relatively uncommon, affecting approximately 2 people per 100,000, but excessive alcohol consumption is linked to as many as 36% of these cases: 61% of HCC were attributable to HCV, 13% to HBV, and 18% to heavy alcohol drinking.
Alcohol intake of more than 2 drinks per day is associated with a small increased risk of lung cancer.
There is a positive association between alcohol consumption and skin cancer.
Baseline alcohol intake as well as lifetime alcohol consumption were associated with an increased risk of the development of squamous cell carcinoma, basal cell carcinoma, and melanoma in men: in women, but the association wasn’t as strong as that seen in men.
Any alcohol intake is associated with the development of malignant melanoma.
There is a statistically significant increases in risk for cancers of the stomach, colon, rectum, liver, female breast, and ovaries.
Heavy alcohol consumption may increase the risk of stomach cancer in heavy smokers.
Alcohol consumption equivalent to 2 or more drinks per day increases risk of endometrial cancer in postmenopausal women.
Alcohol has been suggested as a risk factor for gallbladder cancer.
Evidence suggests that a high intake of alcohol is associated with gallbladder cancer, with men may be at a higher risk of alcohol-related gallbladder cancer than women.
A relatively elevated alcohol intake (of the order of 40 g per day or more) may cause a modest increase of epithelial ovarian cancer risk.
Associations between alcohol consumption and cancers of the ovary and prostate, but only for 50 g and 100 g a day.
Statistically significant increases in risk also exist for cancers of the stomach, colon, rectum, liver, female breast, and ovaries.
Studies show only a weak association between overall alcohol intake and prostate cancer risk, and no association at all between beer and red wine intake and prostate cancer risk.
Alcohol consumption of 50 g and 100 g per day is also associated with cancers of the ovary and prostate.
The Fred Hutchinson Cancer Research Center found that men who consumed four or more glasses of red wine per week had a 50 percent reduction in the risk of developing prostate cancer.
Alcohol consumption is associated with adenocarcinomas and malignant carcinoid tumors.
A 3-fold increased risk in heavy drinkers (80+g ethanol/day) relative to more moderate drinkers and non-drinkers was observed for small intestine cancers.
Maternal alcohol consumption during pregnancy increases the risk of infant leukemia, especially AML.
The risk of an associated cancer is greatest in heavy drinkers: mostly on the order of four or more drinks per day.
There appears to be no increased risk for people consuming up to 30g of alcohol a day, which is approximately 2 alcoholic beverages/day.
There is a modest increase in risk of pancreatic cancer with consumption of 30 or more grams of alcohol per day.
About 7 out of 10 cases of chronic pancreatitis are due to long term heavy drinking.
Chronic pancreatitis is a known risk factor for cancer of the pancreas.
But chronic pancreatitis that is due to alcohol doesn’t increase risk as much as other types of chronic pancreatitis. So if there is a link with alcohol and pancreatic cancer risk, it is only very slight.
Allcohol drinking at the levels typically consumed by the general population of the United States is probably not a risk factor for pancreatic cancer.
The excess risk for pancreatic cancer among alcoholics is small.
There is no association between alcohol use and bile duct cancer.
Allcoholic women are at high risk for in situ and invasive cervical cancer but it is attributed this to indirect, lifestyle-related reasons.
Ductal carcinoma in situ (DCIS) patients and control subjects did not differ with respect to oral contraceptive use, hormone replacement therapy, alcohol consumption or smoking history, or breast self-examination: Associations for LCIS were similar.
Ependymoma-consumption of beer was associated with increased risk in one study, but not in another.
There is no association between alcohol and uveal melanoma.
Light drinking may decrease the risk of nasopharyngeal carcinoma whereas high intake of alcohol may increase the risk.
studies have indicated an increased risk of neuroblastoma with use of alcohol during pregnancy.
Alcohol use is associated with an increased risk of salivary gland cancer.
There is no evidence of a causal relation between behavior risks of tobacco, alcohol or diet and testicular cancer.
Alcohol intake does not affect the risk of developing thyroid cancer.
Alcoholic women are at high risk for cancer of the vagina, as indirect, lifestyle-related reasons, were cited.
Alcoholic women are at no higher risk for cancer of the vulva.
A population based case-control study in Germany found that alcohol reduced the risk of HL for both men and women but more so for men, whose risk was lowered by 53%.
A study of more than 1 million American women found that increasing levels of alcohol consumption were associated with a decreased risk of Hodgkin’s Lymphoma.
Moderate alcohol consumption was associated with a lower risk of renal cell cancer among both women and men.
A study considering more than 1 million American women found that increasing levels of alcohol consumption were associated with a decreased risk of renal cancer.
Compared with nondrinkers, alcohol consumers had a lower risk for non-Hodgkin’s lymphoma overall.
World Cancer Research Fund recommends that people aim to limit consumption to less than two drinks a day for a man and less than one drink a day for a woman: defines a drink as containing about 10–15 grams of ethanol.
