 Heterogeneous lymphoid disorders resulting from a monoclonal proliferation and expansion of immature lymphocytes in the bone marrow, peripheral blood, and other organs.
Heterogeneous lymphoid disorders resulting from a monoclonal proliferation and expansion of immature lymphocytes in the bone marrow, peripheral blood, and other organs.
A heterogeneous disease in which many genetic lesions resulted in the development of multiple biologic subtypes.
Patients with ALL develop symptoms related to the infiltration of blasts in the bone marrow, lymphoid system, and extra major sides, including the CNS and testicles.
The incident rate of ALL in the US is 1.38 per hundred thousand individuals per year.
There are approximately 6550 new cases and 1330 deaths Estimated in 2024.
ALL is the most common pediatric malignancy representing 75 to 80% of acute leukemia among children.
ALL represents approximately 20% of all leukemia is among adults.
The median age of diagnosis for ALL is 15 years with 55.4% of patients diagnosed less than 20 years of age. 28% of patients are diagnosed at greater than 45 years in approximately 12.3% a diagnosed that greater than 65 years.
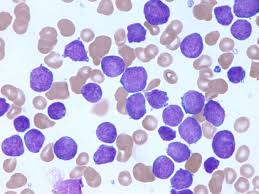
ALL is divided into two major sub types of B cell lineage and T cell lineage with B-ALL accounting for approximately 80% of pediatric cases.
Symptoms include fatigue, lethargy, constitutional symptoms of fevers, night sweats, weight loss, dyspnea, dizziness, infections, easy bruising, or bleeding.
Among children, pain in the extremities or joints may be the only presenting symptoms.
Occasionally lymphadenopathy, splenomegaly, or hepatomegaly may be found.
Chin numbness with facial palsy, may result from cranial nerve or CNS involvement.
Abdominal masses from G.I. involvement are more suggestive of mature B-cell ALL.
Incidence rate in US is 1.8 per 100,000 individuals per year and approximately 6500 new cases in 1330 deaths annually.
The most common pediatric malignancy, which represents 75-80% of acute leukemias among children.
The median age of diagnosis for ALL is 17 years, with 53.5% of patients diagnosed at younger than 20 years of age.
29% of patients are diagnosed at 45 years or older and only 13.7% of patients were diagnosed at 65 years or older.
Accounts for approximately 20% of all leukemias among adults.
WHO classification of acute lymphoblastic leukemia
The WHO classifies ALL as B-lymphoblastic leukemia/lymphoma or T-lymphoblastic leukemia/lymphoma.
B-cell ALL accounts for approximately 80% of pediatric cases.
B lymphoblastic leukemia/lymphoma:
B-lymphoblastic leukemia/lymphoma, not otherwise specified (NOS).
B-lymphoblastic leukemia/lymphoma with recurrent genetic abnormalities ?
B-lymphoblastic leukemia/lymphoma with t(9;22)(q34.1;q11.2); BCR-ABL1 ?
B-lymphoblastic leukemia/lymphoma with t(v;11q23.3); KMT2A rearranged ?
B-lymphoblastic leukemia/lymphoma with t(12;21)(p13.2;q22.1); ETV6-RUNX1 ?
B-lymphoblastic leukemia/lymphoma with hyperdiploidy
B-lymphoblastic leukemia/lymphoma with hypodiploidy
B-lymphoblastic leukemia/lymphoma with t(5;14)(q31.1;q32.3) IL3-IGH
B-lymphoblastic leukemia/lymphoma with t(1;19)(q23;p13.3); TCF3-PBX1
Provisional: B-lymphoblastic leukemia/lymphoma, BCR-ABL-like
Provisional: B-lymphoblastic leukemia/lymphoma with iAMP21
T lymphoblastic leukemia/lymphoma:
Provisional: Early T-cell precursor lymphoblastic leukemia
Provisional: Natural killer (NK) cell lymphoblastic leukemia/lymphoma
The etiology of ALL in childhood as characterized by the acquisition of multiple consecutive genetic alterations in preleukemic cells.
Other genetic disorders that are risk factors for A LL include: Li-Fraumani syndrome, neurofibromatosis, Klinefelter syndrome, Fanconi Syndrom, Bloom syndrome and.ataxia telangiectasia.
Risk factors for childhood ALL included exposure to chemicals found and pesticides and household paint.
Increased incidence among Hispanics, and they have among the lowest survival rates.
African-American children are the least likely to develop ALL, but their survival is worse when compared to children of European and Asian descent.
Accounts for 30% of childhood cancers.
Most common childhood cancer.
About 6000 new cases each year in the U.S.: about 3140 in male patients and about 2880 in female patients.
About 1500 deaths/year.
Most common cause of cancer in children.
Most cases in pediatric ALL are B-cell precursor type.
Bimodal age distribution peaking in children between 3 and 5 years of age and again in persons older than 65 years.
A disease seen across the age spectrum.
Two-thirds of cases in pediatric age group.
Affects 10 in every million young adults aged 15-24 years in the U.S. each year.
Overall incidence of 1.5 per 100,000 persons, with early peak at ages 4-5 years with an incidence of 4-5 per 100,000 and a second gradual increase at about age 50 years with an incidence of 2 per 100,000 persons.
Estimated annual incidence of adult ALL is about one in 100,000.
Childhood ALL has an overall survival of 80% at five years, while adults have an average survival of 35% in patients aged 18-60 years.
Overall ALL survival for children younger than 15 years as improved to greater than 90%, and ALL overall survival and adolescent young adults has improved to 70 to 80%, patients older than 60 years still have poor survival typically down to 20% at five years from diagnosis.
Improvements in ALL survival is due to understanding of the molecular genetics and pathogenesis of the disease, plus the incorporation of targeted agents, the use of allogeneic hematopoietic cell transplantation, and improvements in supportive care.
For all ALL patients, disease relapse remains the major cause of death, with median survival following relapse ranging from less than 10% to approximately 25%.
There is a survival disadvantage for patients between the ages of and and 40 yers compared with both younger and older patients.
Improvements in survival for children and adolescent and young adults with ALL having five year overall survival rates of 89% and 61%, respectively.
Survival rates for adult patients remain low at approximately 20 to 40%.
Median age in most studies is between 25 and 35 years.
80%-90% of ALL patients age 12 years .and younger will survive.
Of the 10 to 20% of patients who relapse, about 40 to 80% of pediatric patients die of the disease within five years.
Relative rare event during late childhood, adolescence and young adulthood.
Prognosis in adolescence and young adulthood appears intermediate.
Survival for infants less than one year age has not seen any improvement over the past 30 years with a six year overall survival rate of 58.2%.
Of all patients who die from the disease most are adults.
With modern intensive treatments outcomes in childhood T-ALL and B-ALL are nearly equivalent.
Survival rates in adults or 30-40% due to poor tolerance of intensive chemotherapy and aspariginase, higher risk of comorbidities and high-risk features predisposing them to disease resistance and relapse.
Approximately 60-80% of adults with ALL achieve complete remission, and 35-40% will survive beyond 2 years.
Minimal residual disease (MRD) greater than 0.1% after inductioninduction is associated with poor survival of approximately 50-60%.
Survival rates are higher in younger adults than in older individuals.
Older patients do less well due to the high risk Philadelphia chromosome being more common in older patients, and older patients are less tolerant of intensive chemotherapy.
Four cytogenetic molecular abnormalities contribute to the worst outcome in adult versus pediatric ALL: Philadelphia chromosome positive ALL, pH-like ALL, Hyperdiploidity, and t(12; 21).
Adults with modern regimens, long-term survival is achieved in 80% of Burkitt leukemia patients, 50% of precursor B cell ALL, 50-70% of pH-positive ALL and 50 to 60% of T-cell ALL.
Most cases the cause is unknown.
Diagnosis requires at least 20% bone marrow lymphoblasts.
Flow cytometry immunophenotyping identifies B or T cell lineage.
B-cell ALL makes up 75-80% of adult cases.
Possible genetic predisposition exists since there is a higher incidence in twins of patients with ALL.
Approximately 75% of adult ALL cases have blasts with the B-cell phenotype and 25% have blasts with the T-cell phenotype.
Unfavorable outcome for T-lineage ALL in both children and adults.
Prognostic value of genetic abnormalities in T-cell ALL less clear then for a B-cell disease.
Up to 20% of adults and 5% of children have the -ABL fusion protein.
The presence of -ABL rearrangement is the most adverse prognostic factor.
ABL rearrangement prognosis not improved with dose intensification.
ABL rearrangement found mainly in common and preB ALL.
IKZFI deletions associated with adverse prognosis in childhood ALL.
Mutations in the IKZF1 gene and other genes encoding kinase activating proteins are important contributors to ALL.
Chromosomal translocations associated with acute lymphoblastic leukemia include: t(12:21)(p13:q22) with ETV6-RUNX1 fusion, t(1:19)(q23:p13) with TCF3-PBX1 fusion, t(9:22)(q34:q11) with BCR-ABL 1 fusion, t(4:11)(q21:q23) with MLL-AF4 fusion, hyperdiploidy and hypodiploidy.
Hispanic children are at higher risk of developing acute lymphoblastic leukemia, but have a poorer survival in children of non-Hispanic ethnic origin.
Incidence of -ABL fusion increases with age and is seen in approximately 3% of children with ALL and 25% of adults with ALL.
Children with -ABL rearrangement had a poor response to prednisone and have high levels of MRD after induction therapy.
BCR/ABL occurs and a quarter to a third of adult patients with ALL.
BCR/ABL abnormalities increases with age.
Presence of Philadelphia chromosome positive ALL is less than 5% in children younger than 10 years, 10-20% in young adults, and as high as 50% on adults older than 60 years with B-cell ALL.
Relative to children, adults with B-cell ALL have a higher frequency of poor-risk genetic changes.
Chemotherapy plus TKI combination regimens are associated with a high complete remission rate of greater than 90%, and the use of MRD studies predict outcomes of patients and can determine whom should receive stem cell transplantation in first remission (Ravandi F et al).
Cure rates for Philadelphia positive ALL in children treated TKIs and chemotherapy has revealed stem cell transplant is no longer essential to cure most children.
Adding TKI to standard chemotherapy improves complete response rate and reduces levels of minimal residual disease, allowing more patients to proceed to transplant and improves overall outcome.
Risk of thrombosis increased and occurs in 1.1-36.7% of cases.
TP53 alterations is associated with high risk of treatment resistance and failure in childhood ALL (Hof J et al).
Glucocorticoids with poor early response indicate in vitro cellular resistance and is an adverse risk factor in ALL.
Response rate increases with increasing glucocorticoid dose.
Some treatment failures related to suboptimal drug dosages in patients with genetic polymorphisms of drug metabolizing enzymes, transporters, receptors or drug targets.
Because the process has wide heterogeneity is essential to differentiate Philadelphia chromosome positive from Philadelphia chromosome negative ALL, and mature Burkitt ALL from the B or T cell precursor ALL.
Microarrays can identify molecular therapeutic targets, gene profiling to predict treated success and relapse rate.
All newly diagnosed patients should have lumbar puncture for cytologic analysis of the CSF fluid.
Risk of relapse includes age of onset, involvement in the cerebrospinal fluid, and initial response to induction therapy.
Treatment approach includes 4 elements: Induction therapy, CNS treatment and consolidation therapy, reinduction, and maintenance therapy.
Induction therapy goal is to produce a morphologic remission and restore normal hematopoiesis.
Induction therapy generally includes 3 systemic agents, a glucocorticoid, vincristine, and L-aparaiginase, it includes intrathecal therapy as well.
In induction therapy the use of anthracycline agents still a matter of debate.
Induction management goals is to induce a complete morphologic remission within 4-6 weeks.
Recent biologic therapy for children who relapse and/or who are refractory include CD19 directed therapy with blinatumomab and chimeric androgen receptor T cells.
Immunotherapies have had the biggest impact in the relapse/refractory setting: Blinatumomab is associated with a 44% complete remission rate and a 33% minimal residual disease negative complete remission rate.; Inotuzumab is associated with an even greater induction of complete remission and MRD negative response with up to 63% of MRD negative rates.
Blinatumomab and Inotuzumab are not associated with prolonged survival, in and of themselves.
Blinatumomab added to conventional. chemotherapy improves the efficacy in advanced newly diagnosed KMT2 A rearranged ALL..
CAR T cells have the highest response rates with complete remission in MRD negative complete remission rates between 80 and 90%.
CAR T cell therapy results in prolonged, durable survival advantage without subsequent therapy in approximately 40 to 50% of patients.
Induction and consolidation in first line treatment of PH-positive acute lymphoblastic leukemia in adults with dasatinib and blinatumab is associated with a high incidence of molecular response and survival (complete response 98%, immediate follow up of 18 months survival 95% and disease free survival was 88%).
Among children, adolescence, and young adults with high and intermediate risk first relapse of B-ALL post re-induction treatment with Blinatumumab compared with chemotherapy, followed by transplant did not result in a statistically significant difference in disease free survival (Brown P).
In patients with relapsed or refractory B-cell acute lymphoblastic leukemia treated with CD19 CAR T cells have noted complete response rates of 6 months of nearly 70%.
CNS therapy is intended to prevent CNS relapse and to reduce systemic minimal residual burden.
The usual management for CNS is achieved by weekly or biweekly intrathecal therapy along with systemic drugs of high dose methotrexate and 6MP.
In children with acute lymphoblastic leukemia (ALL) at risk for central nervous system (CNS) relapse, a higher dose of chemotherapy plus two extra doses of intrathecal therapy during early induction can obviate the need for prophylactic cranial irradiation.
Treatment not only resulted in a negligible rate of CNS relapse but also outstanding cure rate and good quality of life.
CNS relapse in patients who never received cranial irradiation is highly curable, with the recent advent of CAR T-cell therapy.
Most pediatric study groups are moving away from the use of CNS-directed radiation due to the high rates of side effects seen in children, including developmental delays and secondary malignancies.
Intensified chemotherapy treatment of the CNS is an effective and less toxic method of treatment in children with ALL at high risk of CNS relapse, and reinforces the concept that CNS radiation therapy should have a very limited role in the treatment of children with ALL.
Reinduction therapy or delayed we intensification usually uses drugs comparable to those used during induction and consolidation therapy and reduces the risk of relapse.
Once adult patients relapse, the outcome is very poor: complete response rates are only 40% in first relapse, 20% in second, and 10% in third.
The estimated three years survival is less than 10% for patients with a relapse in adulthood.
Combination of high dose intravenous methotrexate and intrathecal chemotherapy without cranial irradiation accepted for protection from CNS relapse in children receiving intensive chemotherapy for non-high risk acute lymphoblastic leukemia. In such patients the rate of CNS relapses is 1.2-6.3%.
A phase III Children’s Oncology Group trial of nearly 2500 children and younger adults with ALL showed that methotrexate in large, consistent doses, rather than gradually increasing doses of standard regimen was more active and preventing relapse and extended survival-suggesting a new standard of care.
Children who do not receive cranial or craniospinal radiation therapy and who have attained 10 or more years of event-free survival can expect a normal long-term survival.
Children who receive radiation have a higher risk for the development of a second neoplasm and a slight excess in mortality.
Overall 5-year survival rate for children is 80-86% and the 5-year event-free survival is 78 to 83%.
Almost all children who remain in remission for 4 years after completion of treatment are considered cured.
5-year event free survival of more than 80% in standard risk patients, 70-80% in those with intermediate risk and about 50% for those at high risk.
Patients with standard risk compose about 30% of patients, those with high risk compose about 20% and patients with high risk disease make up about 50% of such patients.
25% of children with ALL are not cured by first-line treatment.
Children age 1-9 the best outcome.
Durable remissions in children with ALL require about a two-year maintenance therapy of oral 6 mercaptopurine.
Children age 10-20 years ago slightly worse outcome because of a higher incidence of T-cell leukemia, and a lower incidence of favorable genetic abnormalities such as TEL/AML1 and hyperdiploidy.
TEL/AML1 fusion is found in appoximately 25% of cases and is mutually exclusive with hyperdiploidy, and is associated with improved prognosis.
TEL/AML1 formed by fusion of TEL gene on chromosoe 12 and encodes for phosphoprotein of the ETS family of transcription factors, and AML1 gene on chromosome 21, an encoding gene factor fo the core binding factor.
TEL/AML1 fusion inhibits normal activity of the AML1 gene that involves proliferation and differentiation hematopoietic cells and also is associated with high sensitivity to chemotherapy drugs, especially L-asparaginase.
Hyperdiploidy and TEL/AML1 fusion occur mainly in children younger than 10 years.
ALL cells from older children and adults will more resistant to multiple anti-leukemic drugs than are cells from children in the first the decade of life.
Infants less than one year of age and the relatively poor prognosis because of a high incidence of unfavorable immature proB-ALL phenotype and especially the presence ofMLL gene rearrangements (Biondi A).
Infant acute lymphoblastic leukemia is a rare disease and has a poor outcome.
Infants with ALL diagnosed in the first year of life have a prognosis, with a six year survival of 46% and overall survival of 58%.
Infants with a rearrangement of the gene, including histone lysine N methyl transferase 2A (KMT2A) it is found in 75% of infants with ALL, and have the worst outcomes.
T-cell ALL is noted an approximately 15% of childhood cases of ALL.
T-cell ALL cells accumulate less methotrexate and less cytarabine then precursor B-ALL cells (Rots MG).
Approximately 85% childhood ALL is of the B cell lineage, mainly common or pre-B ALL.
ALL subtype with immature cells characterized by CD10 expression, proB ALL, is associated with a high incidence of MLL gene arrangements and poor prognosis.
Mixed lineage leukemia (MLL) gene abnormalities on chromosome 11q23 occurs in approximately 2% of children above the age of one, and is present in approximately 80% of infants with ALL.
Mixed lineage leukemia (MLL) gene abnormalities in infants associated with a poor prognosis.
Mixed lineage leukemia (MLL) gene abnormalities associated with resistance to corticosteroids and L- asparaginase.
Discontinuation of aspariginase associated with significantly event survival.
Mature B- lineage ALL with cell surface immunoglobulins associated with a favorable outcome when treated with non-Hodgkin lymphoma protocols.
Hyperdiploidy is found an approximately 25% children with B- lineage ALL.
Patients with relapsed and chemotherapy refractory pre-B cell ALL have a poor prognosis despite allogeneic hematopoietic stem cell transplantation and bispecific CD19 antibody fragments.
Hyperdiplod cells have an increased tendency to undergo apoptosis and acumulte methotrexate polyglutamates and are sensitive to antimetabolites and L-aspariginase(Kasper her and her and her GJ).
Hyperdiploidy associated with a favorable outcome, especially with extra copies of chromosome 4, 10, or 17 (Heerma NA).
The 5-year event-free survival for adults about 40%, in spite of an initial complete response rate.
Adults older than 55 years of age have a poor prognostic outlook with a probability of survival of 20% at three years, while adolescents and young adults younger than 25 years do much better if treated with pediatric protocols.
Adult acute lymphoblastic outcomes are poor, with long-term disease-free survival rates of 30-40%.
Salvage chemotherapy in adult acute lymphoblastic leukemia has limited success in induction and maintaining a second remission, and overall survival that five years after relapse is as low as 7%.
In adults elevated white counts associated with negative prognostic influence related to a higher tumor mass and proliferation rate.
More than 90% of adults with ALL can achieve remission with multiply chemotherapeutic agents, and more than 40% achieved complete remission reach 5 year overall survival.
Philadelphia chromosome positive adult ALL patients that receive imatinib or other TKI’s during induction have 10% higher complete response rate than those who do not 15% better overall survival rate at 4 years.
Younger adult ALL patients whose leukemia expresses the CD20 antigen, rituximab improves outcomes.
Young adults age 16-21 years of age have a lower event free and overall survival compared to younger patients, and this is in part related to the higher incidence of tea cell atrophic chromosome positive ALL in a lower frequency of tea (12; 21) and hyperdiploidy in this age group.
ALL patients older than 55 years have poorer outcome due to high rate of adverse cytogenetics and increased toxicity of chemotherapy.
Cell surface antigen CD19 is expressed in up to 100% of B-lineage ALL blast cells and CD22 is expressed on up to 90% of B-ALL blasts.
Majority of malignant B cells (up to 95%) in acute lymphoblastic leukemia maintain CD19 and CD22 cell surface expression at high levels.
CD20 is often expressed in adult ALL, but less frequently in pediatric ALL.
T-cell-engaging by specific single-chain antibodies such as CD19 targeted blinatumomab recruit and activate T cells to attack B-ALL cells.
Blinatumomab is highly effective eliminating minimal residual disease as well as relapsed/refractory ALL.
In the BLAST trial patients with hematologic remission but with persistent minimal residual disease (MRD) received blinatumomab to redirect CD3+ T cells to produce lysis in CD19+ B cells: 78% of patients became MRD-negative.
In a phase 2 study of patients with Philadelphia chromosome negative relapsed or refractory ALL who had relapsed within 12 months of initial therapy received this agent by continuous IV infusion for four weeks, followed by a two week holiday for up to five cycles: response rate 43%, relapse free survival 5.9 months, median overall survival 6.1 months.
In a phase III TOWER study the median overall survival was 7.7 months vs. 4 months with standard chemotherapy in patients with Philadelphia chromosome negative relapsed or refractory acute lymphoblastic leukemia
Omitting daunorubicin in older ALL patients may reduce toxicity without comparing results, and for older patients for Philadelphia chromosome positive disease, low intensity TKI’s and steroids can induce prolonged remissions.
In patients with -ABL rearrangement the complete remission rate is 50-80%,slightly lower than patients without this change, but have a 10% overall survival.
In patients with -ABL rearrangement the only curative treatment is stem cell transplant during the first complete remission.
In adults with ALL the 10 year survival rate is 62% for patients who undergo transplantation in the first complete remission, compared with 43% having relapsed or refractory disease at the time of the procedure (Negrin RS et al).
Stem cell transplant commonly used in adults in first remission because relapse rate is 45%-65% vs less than 25% in children.
For B cell ALL specific recurrent chromosomal abnormalities are the(9;22) (-ABL) and mixed lineage gene (MLL) rearrangements which confer poor outlook and the (12;21)(TEL-AML1) are associated with a favorable outcome.
HER2-neu overexressed in about one third of patients with adult B-cell ALL.
Imatinib, the ABL kinase inhibitor, has an overall response rate of 60-70% and a complete response rate of 17-30% in Philadelphia positive patients who failed chemotherapy, but duration of response is short.
Philadelphia chromosome-like ALL occurs in 25-30% of young adults with ALL.
BCR/ABL-like ALL is a B-cell has a gene expression profile similar to those of BCRABL1 ALL but lacking the BCR/ABL1 translocation.
PH-like commonly involves rearrangements, mutations, and copy number alterations affecting tyrosine kinases or cytokine receptor signaling genes such as cytokine receptor-like factor 2 and is frequently associated with loss of IKAROS family zinc finger protein.
the frequency of PH-like ALL peaks in young adults, witha prevalence of nearly 30%, vs 10% in children and 20-25% in adults.
PH-like ALL is associated with a poor prognosis across all age groups.
CRLF2 translocations are found in 60% of cases of PH-like ALL in young adults.
A significant proportion of patient bone marrow specimens do not grow in culture sufficiently for cytogenetic analysis.
Each year approximately 2000 patients become five-year survivors of childhood acute lymphoblastic leukemia.
Mechanisms that induce acute lymphoblastic leukemia include aberrant expression of oncogenes, chromosomal translocations and hyperdiploidy involving more than 50 chromosomes.
Genetic alterations alter regulatory processes that maintains or enhances the ability of cell self-renewal, impair controls of proliferation, block cellular differentiation, and resist apoptosis.
Children who relapse less than 24 months after diagnosis fewer than 10% achieve disease free survival despite intensive treatment including bone marrow transplantation.
Children who relapse more than 24 months after initial diagnosis have a disease free survival of 40% with salvage therapy.
The choice of prednisone vs. dexamethasone for induction therapy in childhood ALL remains controversial in the ALEOP-BFM ALL 2000 trial dexamethasone was associated with a significant reduction in relapse rate, without improvement in overall survival and was associated with a significant increase in treatment related mortality during induction.
Event free survival in childhood ALL was improved in patients with T-ALL with the use of dexamethasone vs. prednisone for induction therapy (ALEOP-BFM ALL 2000 trial).
In adult patients who relapse the response rate is 30% with salvage therapy, with even worse outcome for those over the age of 40 years and a first remission duration less than 1 year.
Treatment in elderly associated with poor results with a 50% complete remission rate with chemotherapy and remission duration of 3-12 months and probability of long term survival below 10%.
Among adults and elderly patients with acute lymphoblastic leukemia, approximately 50-60% will develop a relapsed disease.
Survival is higher in adult patients, at close to 60%, while elderly patients 60 years or greater typically cannot tolerate the intensity of therapy, approximately 30% will die during the induction phase or while in complete remission.
The cure rate with standard chemotherapy for elderly patients with ALL is only 20%.
In elderly comorbid conditions, poor tolerance to chemotherapy, high mortality rate from chemotherapy induction and high frequency of Philadelphia chromosome account or poor prognosis.
Adult lymphocytic leukemia now has cure rates up to 40%.
In adult ALL subsets combining chemotherapy and targeted therapy has increased five-year survival rates in Philadelphia positive ALL from less than 20% to approximately 70%, by using short-term, dose intensive chemotherapy with rituximab.
In adult ALL subset of CD20 positive B lineage disease is improved with rituximab.
Ph+ positive ALL is an aggressive variant with a poor prognosis.
Ph+ positive ALL treated with 300-1000mg daily of imatinib induces a rapid response and median time to clear circulating blasts of only 3 days (Karamlou K).
In a study of Ph+ALL patients a survival rate at 5 years of almost 40% for 59 adult patients treated with imagining and chemotherapy and/ stem cell transplantation (Bassan R).
Hyper CVAD regimen (cyclophosphamide, vincristine, doxirubicin and dexamethasone) 92% of adults achieve complete remission with a 5-year survival of 38%.
HyperCVAD with imatinib mesylate improves response rate for Philadelphia positive ALL.
HyperCVAD in adolescent and young adults with ALL: rates of CR, 5-year CR duration, 5-year overall survival are 98 per cent, and 55%, respectively.
The addition of rituximab to mature B-cell ALL regimens has improved survival rates to 78%.
All protocols use remission induction, followed by intensification, or consolidation, therapy and continuation therapy to eliminated residual leukemic cells.
The use of delayed intensification benefits all risk groups with 5-year event free survival increased the 87% in the standard risk group.
TPMT genotype can modify disease control and toxicity of treatment in children with ALL.
Genes may modify response by altering folate metabolism, steroid response, drug metabolism and transport and detoxification.
Late effects in children occur in more than two thirds of long-term survivors.
In an attempt to reduce late effects of treatment prophylactic cranial irradiation is being replaced by intrathecal and systemic chemotherapy to reduce radiation associated late complications of second malignancies: impaired mental functioning and endocrinopathy.
Two pediatric trials indicated that prophylactic cranial radiation may be omitted: with cumulative risks of isolated central nervous system relapse relatively low at 4% and 3%, respectively (Vilmer E, Manera R), but event free survival rates in these studies were 68.4% and 60.7% respectively.
Prophylactic cranial irradiation improves outcome in T-cell ALL (Conter).
Total Therapy XIIIA study 22% patients with ALL received prophylactic cranial radiation with an overall 5 year survival of 77.65 and cumulative risk of isolated CNS relapse was 1.2%(Pui).
Induction failure occurs in only 2-3% of cases and such cases have clinical and biologic heterogeneity.
Induction failure associated with high leucocyte count, older age, /ABL gene and T cell phenotype.
In adult B-cell ALL refractory HER2 receptor positive patients refractory to treatment have a partial response to trastuzumab of 13%.
In a phase 2 study of adult patients with Philadelphia chromosome negative relapsed or refractory ALL who had relapsed within 12 months of initial therapy received Blinatumobab by continuous IV infusion for four weeks, followed by a two week holiday for up to five cycles: response rate 43%, relapse free survival 5.9 months, median overall survival 6.1 months.
Children with ALL have a high incidence of vetebral fractures after 12 month of chemotherapy associated with reductions in BMD (Alos N et al).
The prognosis for adults with relapsed acute lymphoblastic leukemia is poor.
Adult acute lymphoblastic leukemia: Treatment guidelines and recommendations
ALL is also defined as either standard-risk or high-risk.
Older age is usually associated with poorer outcomes.
Minimal residual disease is a well-established risk factor and predictor to help treatment decisions.
Complete molecular remission after treatment is the main goal of treatment and predicts survival and long-term remission.
Steroid drugs are usually given for 5 to 7 days before primary treatment with chemotherapy.
Standard chemotherapy includes: daunorubicin , doxorubicin, idarubicin and cyclophosphamide, usually with a steroid drug.
Chemotherapy regimens are often given in cycles over 2 induction protocols to induce remission, over 1 to 2 months.
Following remission induction consolidation cycles are given.
Alternatively, is to repeat 2 different intensive chemotherapy cycles, with a total of 8 cycles.
Maintenance therapy, usually consists of daily 6-mercaptopurine and weekly methotrexate for 2.5 to 3 years after primary treatment.
6 to 16 weeks after primary chemotherapy, evaluation of remission status is performed.
Overall CR rate is 83%, and 90% for standard-risk disease and lower for high-risk disease, at about 75%.
Cure rates range from 80 to 90% in childhood.
Cure rates decrease to less than 10% in elderly or frail patients.
Cure rates for adolescent/young patients with ALL remain suboptimal compared with those for children.
Adolescents and young adults, typically from 15 to 40 years benefit from pediatric oriented therapy, with 5-year survival rates with pediatric therapies 67 to 78% , compared to conventional therapy 34 to 41%.
Elderly ALL patients may undergo less intensive therapy to avoid side effects, often based on vincristine (Oncovin) and asparaginase (Elspar) as well as steroids.
In older ALL patients treated with a less intensive protocol had a CR rate of 71%, and early death rate decreased to 15%.
Long-term survival for specific types of ALL, such as Burkitt leukemia or Philadelphia-positive ALL has improved with the tyrosine kinase inhibitor imatinib in combination with chemotherapy.
After ALL patients reach their first CR, they may undergo a stem cell transplant, and it is recommended for all patients with poor early minimal residual disease response.
Standard-risk patients with sustained response may not benefit from an stem cell transplant.
For patients in their second remission or later a stem cell transplant is recommended.
Risk factors for relapse in patients with ALL who have undergone HSCT include hyperleukocytosis and diagnosis with a white count greater than 30,000, cytogenetics associated with poor outcomes, including chromosome 11 translocations and T (9; 22), a short remission ransplant time, more than a first complete remission, and a failed or delayed remission after induction therapy.
Inotuzumab ozogamicin, an anti-CD22 antibody conjugated to calicheamicin, results in better outcomes in patients with relapsed or refractory acute lymphoblastic leukemia than does standard therapy.
Randomly assigned adults with relapsed or refractory acute lymphoblastic leukemia to receive either inotuzumab ozogamicin or standard intensive chemotherapy.
The rate of complete remission was significantly higher in the inotuzumab ozogamicin group than in the standard-therapy group 80.7% vs. 29.4%.
Progression-free survival was significantly longer in the inotuzumab ozogamicin group 5.0 vs. 1.8 months.
The median overall survival was 7.7 months versus 6.7 months.
The most frequent grade 3 or higher nonhematologic adverse events with inotuzumab ozogamicin were liver-related veno-occlusive liver disease.
The rate of complete remission was higher with inotuzumab ozogamicin than with standard therapy, and a higher percentage of patients in the inotuzumab ozogamicin group had results below the threshold for minimal residual disease.
Both progression-free and overall survival were longer with inotuzumab ozogamicin.
Veno-occlusive liver disease was a major adverse event associated with inotuzumab
Blinatumobab is a CD3/CD19 antibody construct for relapsed/refractory ALL.
CAR T-cell therapy is approved for the management of the refractory/relapsed ALL.
Tisagenlecleucel a single infusion of CD 19 CAR therapy provides durable remission with long-term persistence in pediatric and young adult patients with R/R B cell ALL with an overall response rate of 81%.
ELIANA trial assessed the efficacy tisagenlecleucel in children and adult patients with relapsed or refactory B-cell ALL- efficacy demonstrated 81% had a complete remission.
