Third leading cause of death in the U.S.
Second leading cause of death worldwide.
Of the nearly 800,000 strokes in the US each year 87% ischemic in origin, caused by in situ thrombosis, embolism, or systemic hypoperfusion.
It is a time sensitive medical emergency resulting in death of approximately 2 million neurons with each passing minute.
Without treatment the risk of a major stroke in the week after a TIA or minor stroke can be as high as 10%.
Minor stroke is defined as a NIH stroke scale score less than or equal to 5 and accounts for approximately 50% of acute ischemic strokes.
Estimated approximately 25% of ischemic strokes are cryptogenic.
Among patients with acute ischemic stroke in the US, 18.2% have atrial fibrillation and this prevalence increases 40% in patients older than 85 years.
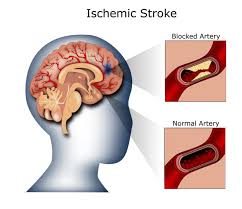
Results from vascular occlusion that impairs cerebral blood flow to the area of the brain perfused by the artery.
Occurs when any artery supplying the brain with oxygen becomes stenosed or occluded, resulting in infarction.
The primary lesion of ischemic stroke is cerebral infarction.
When inadequate supply blood to cerebral tissue occurs, there is initially irreversible loss of tissue function and given enough time infarction with loss of neurons and supportive structures occurs.
Ischemia begins with loss of electrical function and progresses to disturbances of membrane function with calcium influx leading to calcium dependent excitotoxicity, generation of reactive oxygen species, and ultimately destruction of cell membranes and lysis of cells.
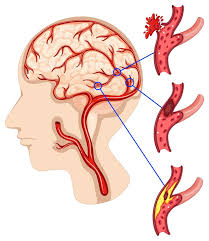
The main causes of acute ischemic stroke are large extra cranial or intracranial vessel high-grade stenosis or occlusion, small vessel disease, cardioembolism, and in a small percentage of patients, varying miscellaneous causes.
Embolism is the most common mechanism of stroke.
Embolism is the most common mechanism of stroke.
The majority of emboli are blood clots generated from the heart due to cardiac disease or associated with cardiac disorders: age of fibrillation, valvular heart disease, cardiomyopathy from myocardial infarction or hypertension.
Valvular vegetations from an infected or not infected thrombotic endocarditis may cause cardio embolism.
Less frequentcauses of cardiomyopathy including viral, drug induced, infiltrative, hereditary or idiopathic can lead to low left ventricular ejection fraction, arrhythmia and intracardiac thrombus formation that can cause embolic strokes.
Diverse causes: classic thrombotic or embolic, prolonged hypotension, cardiac arrest before resuscitation.
Right to left shunting most commonly seen from patent foramen ovale or from congenital heart disease may lead to paradoxical embolism from the venous circulation.
Artery to artery embolism occurs when thrombus, usually that is associated with a atherosclerotic plaque or at the sites of arterial dissection is dislodged from a large vessel wall to flow distally and lodge in smaller downstream vessels.
Rarely other materials than thrombus can embolize to cause stroke.
Large blood vessel disease commonly causes stroke and is most commonly found in the proximal cervical internal carotid arteries, but often more distal in the internal carotid arteries, in the aorta, the vertebral and basilar arteries, or intracranially, may cause strokes.
Arterial dissection of the internal carotid vertebral arteries is the mix most common cause of large vessel disease.
Arterial dissection is a common cause of stroke in young patients without atherosclerotic risk factors and with certain predisposing conditions.
Dissection may be caused by major trauma or by minor trauma from coughing, vomiting, or chiropractic manipulations.
Some lesions that affect the integrity of the connective tissue may lead to dissection of such arteries.
These arterial dissections may occur without apparent provocation.
Small vessel disease can cause small deep strokes to create lacunar strokes.
Small penetrating arteries are most vulnerable to chronic hypertension and are most commonly affected.
Lacuna infarction is common in certain sites: posterior limb and genu of the internal capsule, the basis pontis, thalamus and the cerebellum.
The left atrial appendage has been implicated is a major source of emboli in more than 90% of ischemic strokes
Occurs when an artery supplying the brain becomes occluded and results in the death of brain tissue and focal neurologic deficit.
Most cases are caused by an embolic or thrombotic occlusion of an intracranial arteries.
Strokes that occur in patients with atrial fibrillation associated with increased mortality and morbidity, severe disability and a greater rate of stroke recurrence and longer hospitalization.
Usual evaluation includes magnetic resonance imaging of the brain, MRI angiographyof the neck, echocardiography, and electrocardiography monitoring, and in many cases a transthoracic echocardio graphic study to look for structural abnormalities and screening bloodwork that includes a blood and platelet count, INR and partial thromboplastin time.
In younger patients with a stroke, a more extensive search for a coagulation disorder is performed.
After a complete evaluation the likely stroke etiology can be established in 80-85% of patients, but in 15-20% it remains elusive, cryptogenic.
Previously ask many as 40% of acute ischemic strokes have no identifiable cause and were categorized as cryptogenic.
Cryptogenic strokes occur in patients who are younger than those with identifiable causes of ischemic stroke, and are less severe, and less disabling, and less likely to recur than other ischemic strokes.
Approximately 15% of AIS is preceded by TIA.
The greatest risk for post-TIA stroke is within the first 48 hours, and the risk continues for 3 months.
If reduction in blood flow becomes sufficiently severe cellular changes occur that lead to a infarction.
With a fall of cerebral blood flow by approximately 50% patients will remain asymptomatic, but with a further fall reversible neuronal dysfunction occurs, leading to ischemic symptoms with findings depending upon the location of the ischemia.
If flow can be restored rapidly, neuronal function returns without infarction and the patient will have suffered from a transient ischemic attack.
If, however, low flow ischemia lasts long enough irreversible tissue injury occurs leading to cerebral infarction or ischemic stroke.
The time from onset of symptoms until the onset of irreversible tissue injury depends on the magnitude and duration of the drop in cerebral blood flow.
Infarction may occur within minutes in the core of the lesion, and it may occur much later in the periphery.
The core is the area of the brain that is probably irreversibly infarcted, while the penumbra is the area of the brain around the core that grows overtime and may be salvageable.
The duration of delay until complete infarction varies from minutes to hours, before the window of opportunity to minimize the stroke volume closes.
Ischemia leads to release of excitatory amino acid neurotransmitters, influx of calcium, generation of free oxygen radicals, membrane depolarization, and subsequently loss of membrane integrity.
Symptoms include: numbness of the face, hands, or leg, with the without weakness
Paralysis
Slurred speech
Dizziness
double vision
Hemianopnia
transient monocular blindness
Imbalance
aphasia
confusion
head pain
Blurred vision.
Salvage of an ischemic penumbra is the basis for recanalization therapy to minimize the effects of an acute ischemic stroke.
An ischemic penumbra is defined as brain tissue with reduced blood flow that is at risk for infarction if flow is not reestablished.
Neurons, astrocytes and vascular structures interact as a neurovascular unit and disturbance of complex signaling between components of the neurovascular unit play an important role in ischemic brain injury.
Matrix metalloproteinase 9 becomes upregulated with ischemia and may contribute to break down of the blood-brain barrier and hemorrhagic transformation.
Oxidative stress and inflammation are triggered by ischemia and contribute to cell injury and infarction.
Risk higher among men than among women, among blacks than whites, and in older than in younger age groups.
Referred to as a brain attack.
Mortality rate of 20-50%.
30 day mortality for ischemic stroke 8-12% for people 45-64 years of age (Rosamond WD et al).
Framingham Heart Study revealed that among survivors of ischemic stroke 65 years or older evaluated 6 months after the event, 50% had some evidence of hemiparesis, 30% of patients were unable to walk without assistance, 19% had aphasia and 26% were institutionalized ().
Median age 65 years.
Migrainous infarct is estimated to account for 1.2-14% of all ischemic strokes in patients under the age of 45.
Neurological defect is generally maximal of the time of onset.
Approximately 5% present with seizures and up to 30% have a headache.
Risk factors include TIA’S, previous stroke, coronary artery disease and atrial fibrillation.
The classical presentation of neurologic deficit is rapid onset and localized to a single cerebral arterial vascular territory.
AIS evaluation includes a blood sugar to exclude hypoglycemia and brain imaging is required to rule out intracerebral hemorrhage by non-contrast CT:MRI can also be used.
Aim of acute stroke treatment is recanalization of occluded arterial blood vessel and reperfusion of the ischemic brain region.
A noncontrast CT that shows no other explanation for an acute neurologic deficit is sufficient to diagnose AIS on initial imaging.
Evaluation by CT is for the presence of hemorrhage or other alternative non-stroke diagnoses that might explain the presentation, signs of infarction, and evidence of site of vascular occlusion.
Hemorrhage appears it’s on head CT and its presence is an absolute contraindication for intravenous thrombolytic therapy.
Early signs of inform include loss of gray – white differentiation due to decreased density in gray matter structures.
Over time there is sulcal effacement due to tissue swelling, and other signs of mass effect, and hypodensity are seen.
In early onset of acute ischemic stroke CT may be normal.
MRI is more sensitive for the early identification of AIS.
MRI diffusion weighted imaging is nearly 100% sensitive in identifying acute infarction.
MRI angiography can demonstrate flow or stenosis or occlusion in arteries of the chest, neck, and head.
Initial diagnosis imaging should be performed quickly.
Familiarity with stroke warning signs in the US is lacking with black and Hispanic patients compared with the general population, putting them at higher risk of prehospital delays in seeking medical assistance.
Noncontrast CT, diffusion weighted MRI and perfusion CT measurements are used to define ischemic brain tissue evaluating the extent of ischemic changes and the potential of salvageable tissue.
Treatment:
Acute treatment of stroke is directed at early reperfusion with intravenous thrombolysis or endovascular thrombectomy to provide optimization of hemodynamic status with management of fluid volume, blood pressure, and cardiovascular status.
Endovascular clot retrieval is a highly effective treatment for patients with acute ischemic stroke with a large cerebral vessel occlusion withi approximately 80% rate of successful vessel recanalization.
For every 2 to 4 patients treated an additional patient achieves functional independence.
Despite recanalization, 50 to 60% of patients undergoing endovascular therapy for a stroke due to a large vessel occlusion die or remain disabled at 90 days.
Two treatments are considered standard of care in acute ischemic stroke management: intravenous alteplase administered within 3-4.5 hours after symptom onset and endovascular therapy initiated within six hours of symptom onset.
Among patients with acute ischemic stroke treated with intravenous alteplase the use of NOACs within the preceding seven days, compared with no use of anticoagulants, was not associated with significantly increased risk of intracranial hemorrhage.
Among patients with minor non-disabling, acute ischemic stroke presenting within 4 1/2 hours of symptom onset, dual antiplatelet therapy was not inferior to intravenous Alteplase with regard to excellent functional outcome at 90 days (ARAMIS investigators).
Randomized controlled studies have shown that endovascular thrombectomy alone achieves outcomes that may be non-inferior to outcomes achieved with combined intravenous thrombolysis plus endovascular thrombectomy for patients with acute ischemic stroke and large vessel occlusions.
In patients with acute ischemic stroke due to large vessel occlusion presenting within 24 hours of time last known to be well, and who had achieved near complete to complete reperfusion with endovascular reperfusion thrombectomy, adjunctive intra-arterial tenecteplase did not significantly increase the likelihood of freedom from disability at 90 days (POST-TNK investigators).
Among patients with acute ischemic stroke due to large vessel, occlusion, adjunct intra-arterial urokinase after near complete or complete reperfusion by endovascular thrombectomy did not significantly increase the likelihood of survival without disability at 90 days (POST-UK investigators).
Among patients with acute ischemic stroke, due to large vessel occlusion undergoing endovascular thrombectomy, the addition of methylprednisolone did not significantly improve the degree of overall disability (MARVEL trial).
Among patients with large, ischemic strokes, endovascular thrombectomy results in better functional outcomes than standard medical care (SELECT2 investigators).
The benefit from endovascular therapy is greater when employed earlier.
Guidelines recommend consideration of endovascular therapy when there is inclusion of the M1 segment, that is the main trunk, of the middle cerebral artery or internal carotid arteey and when findings indicate the size of the infarct area is not large.
Approximately 54% of patients who experience severe strokes have functional dependence or die, and among those who survive, approximately 72% have some degree of disability.
In a study of anterior circulation stroke, Endovascular Treatment alone was neither superior nor not inferior to intervenous aleplase followed by endovascular treatment with respect to functional outcomes at 90 days.
Intravenous alteplase at a dose of 0.9 mg per kilogram of body weight over 60 minutes with the first 10% of the dose given as a single bolus over one minute, within 4 1/2 hours after the onset of stroke reduce his disability from acute ischemic stroke.
IV alteplase benefits patients with disabling stroke regardless of their NIHSS score.
Among Chinese patients with mild posterior circulation stroke, who did not receive thrombectomy, alteplase administered 4 1/2 to 24 hours after stroke, resulted in high frequency of functional independence at 90 days than standard medical care.
Alteplase is not recommended for patients with non-disabling stroke and patients with an NIHSS score of 0 to 5, for those with bleeding risk that is excessive, or a CT evidence of irreversible injury exists.
Among patients with ischema stroke treated within 4.5 hours after symptom onset reteplase was more likely to result an excellent functional outcome than Alteplase (RAISE clinical trials).
Although beneficial overall, many patients with proximal large vessel occlusion of the middle cerebral artery stem and internal carotid artery do not respond to IV tPA.
All patients with presenting within six hours of onset with significant functional defects in large vessel occlusion without a large established stroke, and without contraindications should be considered for endovascular thrombectomy.
Mechanical thrombectomy is associated with a 20 to 27% absolute increase in the rate of functional independence compared with patients not treated with thrombectomy.
Modern thrombectomy with stent retrievers and direct aspiration systems have enabled high levels of reperfusion to be achieved an acute ischemic stroke from large vessel occlusion, still more than half of patients do you not survive free of disability due to the rapid evolution of cerebral infarction and periprocedural complications.
Before administering alteplase noncontrast CT of the brain scan is necessary.
Alteplase is contra indicated with coagulopathy and blood pressure must be lower than 185/110 mmHg before and during infusion and lower than 180/105 mmHg for at least the first 24 hours afterward.
The benefit of intravenous alteplase is time dependent.
The magnitude of benefit of both treatments is directly related to recanalization speed that is achieved.
Treatment for AIS is guided by the time from onset, the severity of neurologic deficit, and findings on neuroimaging.
The severity of neurologic deficit is measured by NIH stroke scale, on which scores range from 0-42, with low numbers indicating a milder deficit.
Deficit severity is characterized by non-disabling or disabling manifestations that would prevent performance of activities of daily living or return to work.
TPA time window 3 hours from onset of stroke, after that the increased risk of bleeding outweighs benefits of thrombolytic therapy.
TPA remains the only approved drug for acute ischemic stroke.
The standard tPA dose for acute stroke patients is 0.9 mg/kg.
TPA approval was based on the results of the 1995 National Institute of Neurological Disorders and stroke tPA trial: significant improvement in function outcome at 90 days was found if TPA was given within three hours of symptoms, however no improvement at 24 hours was seen and there was a 6.4% increased risk of symptomatic intracranial hemorrhage.
Of patients with acute ischemic stroke only 2-8% receive TPA therapy.
IV TPA compared with no reperfusion has been demonstrated in randomized trials to improve three month functional outcomes after acute ischemic stroke, and one year-1.5 year functional outcomes.
In a retrospective study of 61,426 patients with acute ischemic stroke treated with intravenous tissue plasminogen activator, longer door-to-needle times were significantly associated with higher all-cause mortality at one year and a higher likelihood of all-cause readmission at one year (Man S).
Intravenous alteplase given within 4.5 hours after onset of stroke is the only reperfusion therapy with proven efficacy in patients with AIS.
Alteplase is less effective att opening proximal occlusions of the major intracranial arteries, which account for more than one third of cases of acute anterior circulation stroke.
In a prospective study of 575 patients with AIS and visible intracranial thrombus on CT angiogram, thrombus recal thrombus recanalization occurred in 30.4% of patients within six hours of intravenous alteplase administration, and 13.3% of patients who did not receive alteplase(Menon BK).
About one third of patients with intravenous alteplase and occlusion of the internal carotid artery terminus have early recanalization, and without revascularization the prognosis is poor.
The use of intravenous recombinant tissue plasminogen activator (t-PA) results in more than half of the patients treated do not recover completely or die.
The gaol is t-PA therapy is to be given by 60 min. after stroke onset.
Intravenous t-PA is the only effective treatment to improve the outcomes for acute ischemic stroke.
Recanalization rates within 24 hours after the administration of intravenous TPA are low when the occlusion involves a large intracranial artery: with 14% for internal carotid arteries and 55% for middle cerebral arteries (Rha JH, Saver JL).
IV tissue plasminogen activator administered within 4 1/2 hours after the onset of acute ischemic stroke improves outcomes.
Endovascular mechanical treatment is capable of removing large, proximal clots and result in higher rates and reperfusion than intravenous t-PA alone.
Mechanical thrombectomy is achieved by passing an intra-arterial catheter from peripheral puncture into an intracranial artery and removing an including thrombus by ensnaring it or by suction.
Mechanical thrombectomy within 6 hours after the onset of am AIS is another first line treatment for patients.
Guidelines recommend use of endovascular thrombectomy in the treatment of acute ischemic stroke for patient to have occlusion of the internal carotid artery or proximal middle cerebral artery with at least moderately severe presenting stroke deficits and absence of evidence of widespread establish infarction on brain imaging.
CHOICE study demonstrated the use of Alteplase following thrombectomy is more effective than Alteplase alone in Acute ischemic stroke.
In patients with acute ischemic stroke eligible for intravenous thrombolysis within 4.5 hours after stroke onset tenecteplase was not inferior to alteplasei with respect to excellent functional outcome at 90 days and had a similar safety profile (Meng X).
This recommendation applies when endovascular treatment can be initiated within six hours of symptom onset.
Controlled studies have shown a benefit of mechanical thrombectomy performed more than six hours after the onset of stroke in patients with an occlusion of the intracranial internal carotid artery or the first segment of the middle cerebral artery.
Randomized trials have consistently shown that mechanical thrombectomy with or without intravenous thrombopolysis using recombinant tissue plasminogen activator (rt-PA) can improve the outcome in patients with acute stroke due to large vessel occlusion.
Intravenous thrombplysis prior to mechanical thrombectomy is recommended by national guidelines for patients with large vessel occlusion, within 4.5 hours of symptom onset.
Meta-analysis of five randomized clinical trials reported outcomes following mechanical thrombectomy did not differ significantly between patients receiving and not receiving intravenous thrombolysis.
Randomized studies have demonstrated that endovascular mechanical thrombectomy leads to a better functional outcome compared with medical therapy in patients with acute ischemic stroke due to large vessel occlusion.
Mechanical thrombectomy strategies involves the use of second generation devices such as stent retrievers or contact aspiration catheters as an initial therapy for a stroke.
Among patients with acute ischemic stroke due to large vessel occlusion, and initial thrombectomy technique consisting of contact aspiration and stent retriever combined did not significantly improve the rate of near total or total reperfusion at the end of the endovascular procedure as compared with stand retriever alone.
For the foreseeable future, thrombolysis will remain the most common and widely applicable therapy for stroke treatments because the majority of patients with acute ischemic stroke do not have large artery clots approachable by endovascular thrombectomy.
In a randomized study of patients with acute ischemic stroke receiving intravenous t-PA alone or endovascular thrombectomy with a stent retriever within six hours of the onset of stroke: The latter group had improved functional outcomes at 90 days (Saver JL et al).
Mechanical thrombectomy with a stent retriever recommended for patients with occlusion of the internal carotid artery or proximal middle cerebral artery with at least moderately severe presenting stroke deficits and absence of evidence of widespread establishment of infarction on brain imaging, when endovascular treatment can be initiated within six hours of symptom onset.
Mechanical thrombectomy with a stent retriever is also recommended for acute ischemic stroke patients presenting at later times.
In the above study patients with acute ischemic stroke due to large vessel occlusion, emergency neurovascular thrombectomy with stent retriever was safe and effective in achieving reperfusion and reducing disability and increased the number of patients with functional independence three months after stroke.
Endovascular thrombectomy is a safe and effective treatment for appropriately selected patients with acute ischemic stroke up to 24 hours after symptom onset.
There are multiple constraints to intravenous t-PA and include unresponsiveness of large thrombi to rapid enzymatic digestion, narrow window time for administration, risk of cerebral and systemic hemorrhage.
In patients with occlusion of the intracranial internal carotid artery or the first segment in the middle cerebral artery and intravenous t-PA results in early reperfusion in only 13-50% patients.
TPA given intravenously for acute ischemic stroke carries the risk of symptomatic intracranial hemorrhage.
Intravenous t-PA for stroke is associated with potentially life-threatening complications in 2.4-8.8% of cases.
In a randomized study involving 500 patients in the Netherlands assigned to intraarterial thrombolytic therapy/stent or to usual care alone: in patients with acute ischemic stroke caused by a proximal occlusion of the anterior circulation, intrarterial treatment administered within 6 hours was safe and effective (MR CLEAN Investigators).
In the CHOICE trial intra-arterial administered thrombolysis using Alteplase immediately after successful thrombectomy had an 18% increase in excellent outcomes compared with placebo.
In the above study there were no significant differences in mortality or occurrence of symptomatic intracerebral hemorrhage, but there was an absolute difference of 13.5% in the rate of functional independence.
Each minute following an acute ischemic stroke approximately 1.9 million neurons die (Saver).
MRI and CT perfusion studies in patients with acute ischemic stroke suggest ischemic areas of the brain may in some cases remain viable for as long as 24 hours, with potential for restoration of normal function with reperfusion (Darby DG et al).
Only aspirin and possibly thrombolytics have shown a benefit in outcome.
Aspirin, provides greater benefit for women than men in the primary prevention of ischemic stroke.
Among patients with mild-moderate acute non-cardio embolic ischemic stroke the risk of stroke or death within 30 days was lower with ticagrelor-aspirin than aspirin alone, but the incidence of disability did not differ significantly between the two groups (Johnston SJ).
An international multicenter registry study observed a substantial reduction in 30-day and 90-day stroke risk after a TIA presentation in patients on statins, if they had evidence of carotid stenosis, but not otherwise (Merwick A et al.).
Statins reduce stroke risk when initiated months after transient ischemic attack (TIA)/stroke.
Statins reduce early vascular events in acute coronary syndromes.
In acute symptomatic carotid stenosis, statin pretreatment was associated with reduced stroke risk supporting the hypothesis that statins started acutely after TIA symptom onset may also be beneficial to prevent early stroke.
The initiation of thrombolytic therapy should be as soon as possible, delay is justifiable for brain imaging studies and a few laboratory tests.
Risk of withholding rt-PA greatly exceeds the risk of giving it.
One in three of all patients with stroke come to the emergency department within the appropriate time window and meet the requirements for acute thrombolytic therapy.
Most common reasons that patients do not qualify for tPA therapy is that they do not present to the emergency department in time to receive it.
Effectiveness of TPA is time-dependent with treatment beyond 4.5 hours after stroke onset does not result in improve clinical outcome (Lees KR et al).
Endovascular treatment for acute stroke consists of endovascular administration of fibrinolytic medications at the site of vascular occlusion, and is often given beyond the three-hour approved time window for intravenous TPA.
PROACT II (Prolyse in Acute Severable Thromboembolism) is the only randomized trial demonstrating clinical efficacy and improve recanalization compared with control treatment in a 0-6 hour time window(Furlan A et al).
It is suggested that small doses of subcutaneous heparin be used during 24 hours after thrombolytic therapy to avoid the development of deep venous thrombi.
Low molecular weight heparin should not be used since it increases the risk of extracranial bleeding.
Anticoagulants used alone or with antiplatelet agents are not superior to antiplatelet drugs used alone.
Increased body temperature is a predictor of adverse outcome after stroke.
A decrease of 0.3 ‘C in body temperature can lead to a 10-20% relative risk reduction in poor outcome for patients with acute stroke.
Up to 30% of survivors will have a subsequent stroke within 5 years and 18% of such events will be fatal.
Risk of myocardial infarction following acute stroke is 5% in the first year and greater than 3% annually for 10 years.
The most frequent causes of death after ischemic stroke are cardiovascular and respiratory diseases.
Increased left atrial volume, equal or greater than 28 mL/m2, is present in about 75% of with first ever ischemic stroke.
Increased left atrial volume more prevalent in older patients and in those with higher number of cardiovascular risk factors.
Increased left atrial volumes increased in all subgroups of ischemic stroke patients but particularly in the cardio embolic group, at 94% (Fatima).
Seizures are the presenting feature in 2-33% of ischemic strokes.
Corticosteroids have no clinical benefits and their use cannot be supported.
MRI studies have a greater overall sensitivity for acute stroke particularly, for the detection of acute ischemic stroke.
Diagnosed with MRI in 46% of patients, but with CT in only 10% of patients.
Endovascular technics to remove intra-arterial thrombus include the Merci Concentric Retriever and the Pnumbra aspiration system are designed to remove the thrombus within eight hours of stroke onset.
In a randomized study of anterior circulation strokes undergoing mechanical embolectomy or standard of care with MRI or CT scan identified favorable penumbral patterns on neuroimaging did not identify patients who benefit from this procedure (Kidwell CS et al).
Endovascular thrombectomy is presently standard treatment for patients who have an acute ischemic stroke due to large vessel occlusion in the anterior cerebral circulation, and when the procedure is available and performed in a timely fashion.
In a randomized study of patients with acute ischemic stroke from a large vessels occlusion endovascular thrombectomy alone was not inferior with regard to functional outcome to endovascular thrombectomy preceded by intravenous alteplase administered within 4.5 hours (Yang P).
Among patients with large vessel occlusion acute ischemic stroke undergoing endovascular thrombectomy treatment with intravenous tirofiban a platelet glycoprotein IIb/ IIIa inhibitor compared with placebo, before endovascular therapy resulted in no significant difference in disability severity at 90 days, and findings did not support the use of intervenous anti-platelet agents before endovascular thrombectomy for acute ischemic stroke.
No device for removing intra-arterial thrombotic material has been proven clinically effective compared to IV TPA.
Recanalization occurs in 46% of cases with intravenous TPA while greater than 80% of patients treated with endovascular treatment recanalize.
Recanalization is not invariably associated with favorable clinical outcome.
In a randomized study of 362 patients with acute ischemic stroke treated within 4 1/2 hours with endovascular therapy, or intravenous TPA: At 3 months 30.4% of the endovascular therapy group and 34.8% of the intravenous TPA group were alive without disability (Ciccone A et al).
Among patients with anterior circulation stroke that could be treated within eight hours of the symptom onset a stent retriever mechanical thrombectomy reduced the severity of stroke disability and increased functional independence (REVASCAT Trial Investigators).
Interventions for improving upper extremity function after stroke reveals that there is no high quality evidence for the superiority of any practice intervention including the amount and content of motor training.
With acute anterior circulation large vessel occlusion, endovascular therapy with thrombectomy is the first line treatment.
In persons with stroke with occlusion of medium or distal vessels endovascular treatment does not result in lower level of disability or a lower incidence of death and best medical treatment alone (DISTAL investigators).
In a study of a large cerebral infarctions there were better functional outcomes with endovscular fibrinolysis therapy than with medical care alone but there were more associated intracranial hemorrhages (Yoshimura S).
Therapy to lower serum lipid levels with statins is recommended after a transient ischemic attack or ischemic stroke of atherosclerotic origin.
The Stroke Prevention by Aggressive Reduction in Cholesterol level (SPARCL) trial shows 16% lower incidence of recurrent stroke with statins than with placebo in patients with stroke and no known coronary heart disease.
In this study patients with carotid stenosis, there was a 33% lower incidence of stroke in the atorvastatin group than in the placebo group.
In this study patients who reached the level of low density lipoprotein cholesterol of less than 70 mg/dL had a 28% lower relative risk of stroke in those who reach the level of 100 mg/dL.
After an ischemic stroke with evidence of atherosclerosis, patient to head to target LDL cholesterol level of less than 70 mg/dL had a lower risk of subsequent cardiovascular events in those who had a target range of 90 mg-110 milligrams per deciliter.
Studies suggest that the risk of stroke is 20% lower for every reduction of 39 mg/dL in the LDL cholesterol level.
Clinical benefit is measured with the use of a modified Rankin scale with scores ranging from 0 to 6 (death); A score of one indicates in ability to carry out all of usual duties and activities, a score of two indicates an inability to carry out all normal activities but inability to look after wins on affairs without assistance.
Tenecteplase is a tissue plasminogen activator that is more fibrin specific and more resistant to plasminogen activator inhibitor and has a longer plasma half live than alteplase so that it can be given as a single intravenous bolus.
Tenecteplase therapy initiated 4.5 to 24 hours after stroke onset in patients with occlusion of the middle cerebral artery or internal carotid artery, most of whom had undergone endovascular thrombectomy, did not result in better clinical outcomes than those with placebo (TIMELESS investigators).
In a Chinese study: patients with basal artery occlusion approximately 1/3 of whom received intravenous thrombolysis, endovascular thrombectomy within 12 hours after stroke onset lead to a better functional outcome at 90 days than best medical care and was associated with procedural complications and intracerebral hemorrhage.
Argatroban a selective thrombin inhibitor, directly inhibits free and clot associated thrombin, as well as thrombin induced events, and is widely used to treat acute ischemic stroke, particularly in Asian countries.
Among patients with acute ischemic stroke treatment with argatroban plus intravenous alteplase compared with alteplase alone did not result in a significant grade likelihood of excellent functional outcome at 90 days.
In patients with an acute ischemic stroke, treated with intravenous thrombolysis within three hours after symptom onset, adjunctive treatment with intravenous argatroban or eptifibatide did not reduce post stroke disability and was associated with increased mortality (Barrett AD).
In patients with acute stroke, and a large infarct of unrestricted size, thrombectomy plus medical care, results in better, functional outcomes and lower mortality in medical care alone, but leads to a higher incidence of symptomatic intracerebral hemorrhage.
Prehospital blood pressure reduction trial did not improve functional outcomes in patients with in differentiated acute stroke.
Fever has been demonstrated to occur in 90% of patients with stroke within seven days and it is associated with secondary brain injury and worse outcomes.
For each 1°C to increase in temperature, the odds of poor outcome increased by 2.2
Short term mortality at odds and increase by 2.2 in a patient with the ischemic stroke experience his fever within 24 hours.
In patients with acute vascular brain injury, preventive normothermia effectively can reduce fever burden, but does not improve functional outcomes (INTREPID study group).
