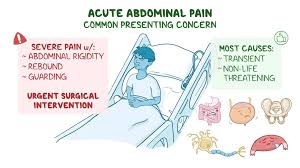
 Acute abdominal pain refers to the sudden onset of severe pain in the abdominal area.
Acute abdominal pain refers to the sudden onset of severe pain in the abdominal area.
Acute abdominal pain is one of the most common symptoms in individuals presenting to the ED and accounts for 5 to 10% of all emergency department visits.
Acute abdominal pain can be caused by a wide range of conditions, some of which may require immediate medical attention.
Here are some potential causes of acute abdominal pain:
Appendicitis-Inflammation of the appendix, often presenting as pain starting near the navel and then moving to the lower right abdomen, sometimes accompanied by fever, nausea, or vomiting.
Gallstones-These can cause a blockage in the bile duct, leading to intense pain in the upper right abdomen, often after eating fatty meals.
Pancreatitis-Inflammation of the pancreas can cause severe pain in the upper abdomen, often radiating to the back, with nausea and vomiting.
4. Gastroenteritis-An infection or inflammation of the stomach and intestines that can lead to cramping pain, diarrhea, and vomiting.
Diverticulitis-Inflammation or infection of pouches (diverticula) in the colon, typically causing pain in the lower left abdomen.
Bowel Obstruction-A blockage in the intestines that can cause cramping pain, vomiting, and the inability to pass gas or stools.
Peptic Ulcers-Open sores that develop on the inside lining of the stomach or upper small intestine, causing burning pain.
Ectopic Pregnancy-A pregnancy that occurs outside the womb, often in a fallopian tube, which can cause severe pain and bleeding.
Renal Colic-Pain caused by kidney stones, typically intense and located in the flank or lower back, radiating to the groin.
Abdominal Aortic Aneurysm-A life-threatening condition where the large blood vessel supplying blood to the abdomen, pelvis, and legs balloons out, potentially causing sudden and severe pain.
It is essential to seek medical evaluation for acute abdominal pain, especially if it is severe, persistent, or associated with other symptoms like fever, vomiting, jaundice, or altered bowel habits.
Necessary exams and tests, such as blood tests, imaging studies, or endoscopy, to diagnose the underlying cause and determine the appropriate treatment.
Acute abdominal pain can be localized or diffuse.
Abdominal pain may be associated with a perforated viscous, peptic ulcer disease, mesenteric ischemia, acute cholecystitis, appendicitis, diverticulitis, pancreatitis, and intraabdominal hemorrhage.
Timely diagnosis is required for intraoperative surgical correction.
During the work up for abdominal pain, the use of analgesia is controversial.
Some investigators believe the administration of analgesia will alter clinical findings and ultimately delay the diagnosis.
However, most clinicians judiciously use analgesia during the evaluation, and the administration of pain medication does not appreciably alter the diagnosis or the time to intervention.
A number of randomized control studies revealed that the administration of analgesia doe not substantially altered the diagnosis accuracy.
CT angiography with administration of intravenous contrast material of the abdomen and pelvis is the primary imaging technique used to assess acute abdominal pain in non-pregnant adults seen in the emergency department.
Contrast enhanced CT angiography can identify sites of intraabdominal inflammation, perforation, or ischemia and has a high positive predictive value for specific abdominal diagnoses.
CT angiogram of the abdomen and pelvis, increases diagnostic certainty, reduces hospital admission rate by 23.8% and leads to more timely surgical intervention.
The use of unenhanced CT to avoid the risks of intravenous administration of contrast material is associated with a 30% less accurate evaluation of acute abdominal pain.
Rapid interpretation of the diagnostic images are required, as a delay of two hours for final interpretation is associated with increased risk of systemic complications and death because of delay in surgical consultation.
Plain abdominal radiography lacks diagnostic sensitivity, and specificity compared to contrast enhanced CT angiography but gross signs with peritonitis and findings of free air can lead to a prompt surgical intervention.
The use of ultrasound in the diagnosis of acute abdomen is based on history and clinical findings and is preferred for the diagnosis of acute biliary disease and appendicitis.
