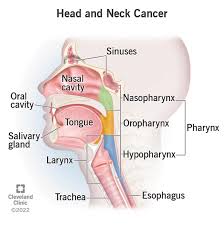
Encompasses a group of malignancies that arise in the mucosal surfaces of the upper aerodigestive tract and include: the oral cavity, pharynx, larynx, and paranasal sinuses, as well as cancers of the major and minor salivary glands.
The pharynx includes the nasopharynx , oropharynx, comprising the tonsillar area, tongue base, soft palate, and posterior pharyngeal wall, and hypopharynx, comprising the pyriform sinuses, posterior surface of the larynx and postcricoid area, and inferior posterior and inferolateral pharyngeal walls.
The pharynx includes the nasopharynx , oropharynx, comprising the tonsillar area, tongue base, soft palate, and posterior pharyngeal wall, and hypopharynx, comprising the pyriform sinuses, posterior surface of the larynx and postcricoid area, and inferior posterior and inferolateral pharyngeal walls.
The nasal cavity and paranasal sinuses include the maxillary, ethmoid, sphe- noid, and frontal sinuses.
Squamous cell cancers are the fourth-sixth most common cancer worldwide.
Squamous cell cancers is more than 90% of head and neck cancers.
More than 70% of all cases are found in developing countries.
Head and neck cancer effects about 66,000 patients and causes 15,000 deaths annually in the US.
Head and neck cancer was the seventh most common cancer and the seventh leading cause of cancer deaths worldwide in 2020.
In 2020 the global annual incidence of HNC was approximately 932,000, and greater than 467,000 deaths.
More than 3/4 of the 65,000+ new cases of head/neck cancer diagnosed each year in the US are related to tobacco and/or alcohol use.
It was the seventh most common cancer worldwide in 2018 with 890,000 new cases in 450,000 deaths.
Accounts for approximately 3-5% of all newly diagnosed cancers.
In the US accounts for 3% of all cancers and over 1.5% of all cancer deaths.
Most patients with squamous cell carcinoma of the head and neck present with locally advanced disease stages III to IVb which is associated with poor survival outcomes.
Decreasing globally, in part due to decreased use of tobacco.
Established risk factors are: smoking, alcohol use, and human papillomavirus.
There is evidence that oral bacteria are risk factor for head and neck cancer development, and identification of bacteria and bacterial complex complexes in the oral microbiome is associated with an associated microbial risk score.
In head and neck cancers, the overall incidence of the synchronous second primary cancer is estimated to be 12%.
Head and neck cancers have a poor prognosis with about 60% five year survival.
Cases of HPV-associated oral pharyngeal cancer, induced primarily by HPV 16, or increasing, predominately among younger people in North America and northern Europe, reflecting a latency of 10-30 years after oral-sex exposure.
Since 1980 declining incidence of -4% and modest improvement in 5 year survival over the last 20 years.
The fraction of head and neck cancer diagnosed as HPV positive oropharyngeal cancers in the US rose from 16.3% in the 1980s to more than 72.7% in the 2000s.
SEER data from 1973-2006 indicated that the overall incidence of head and neck cancer in that time period was stable, but there was a significant improvement in overall survival, particularly for patients with tongue and tonsil cancer.
Improvements in survival may be due to decreased use of tobacco, which has a negative impact on treatment outcome for those who continue to smoke and to an epidemiological shift to a increase in the frequency of HPV related oropharyngeal cancers.
More than 500,000 patients diagnosed worldwide each year, along with 380,000 deaths related to the disease.
Two thirds of cases diagnosed each year occur in developing countries.
Accounts or 3.2% of all new cancers in the U.S. and 2.2% of all cancer deaths.
Lifetime risk 2% for men and 0.6% for women.
3 fold higher incidence in men than women.
More common in African-Americans.
5-year survival is better for whites than for blacks, 61-64% versus 40-52%.
Approximately 40% 5 year mortality rate.
More than 90% of cases squamous cell in origin.
Currently more than 280,000 head and neck cancer survivors in the US.
Arises from successive genetic alterations of mucosa that allows malignant transformation.
Closely linked to immunosuppression and correlates with poorer outcomes.
An immunosuppressing illness with impaired secretion of cytokines as well as dysregulation of immunocompetent cells.
Majority of patients have impaired antitumor responses.
Immune dysregulation in head and neck cancer decreases immunogenicity of the tumor.
At least 10 anatomic subsites affected.
Patients often present with local/regional advanced disease, impairing speech, deglutition, and cosmesis that stem both from the disease and its treatment.
Often amenable to curative treatment when localized, but carries a poor prognosis when it is recurrent or metastatic.
More than half of head and neck cancer survivors are current smokers; 50% continue to smoke following diagnosis.
There is evidence that continued smoking increases mortality in oral cancer.
Recurrent or metastatic disease, or both, develops in more than 65% of patients with squamous- cell cancer of the head and neck.
Heavy tobacco users have a 5-25 fold higher risk of developing such cancers than smokers.
Alcohol increases risk for a greater than 40 pack year smoker and drinks more than 5 alcoholic beverages per day by 40fold.
Alcohol use synergistic with tobacco as a cause of malignancies.
A third of head and neck cancer patients consume more than three alcoholic drinks per day, a behavior that increases the risk of recurrence, depression, and other substance abuse disorders.
Nicotine and polycyclic aromatic hydrocarbons in tobacco are carcinogenic.
Tobacco smoke associated with DNA structural changes, particularly those induced by oxidative changes.
The risk from smoking substantially decreases with time from smoking cessation, but the risk it never reaches the level of a never-smoker.
Patients should be for referred for alcohol and tobacco cessation counseling.
Elderly patients with acid reflux in the United States are 3.47, 3.23, 2.88, and 2.37 times as likely as those without acid reflux to be diagnosed with laryngeal, hypopharyngeal, oropharyngeal, and tonsillar cancers, respectively (MCcoul Ed.)
The cumulative risk at 75 years of age for all upper aero digestive tract cancers was 6.3% for men who continued to smoke, 3.1% for men who stop smoking at around 50 years of age, 1.2% for men who stopped smoking at around 30 years of age and 0.8% among lifelong non-smokers (Bosett C et al).
Long exposure to secondhand smoke, over a period of more than 15 years, is associated with increased risk, particularly of pharyngeal and laryngeal cancers(Lee YC et al).
Significant exposure to alcohol and tobacco associated with mutation of P53 suppressor gene.
Chewing betel quid associated with oral leukoplakia and oral submucosal fibrosis 5:1 in non users.
Betel nut a fruit that is a stimulant chew used by 200-400 million people.
Addition of tobacco to betel nut chewing increases risk of head and neck cancer by additional 3 fold.
Duration and frequency of betel nut use increases risk of developing cancer suggests a dose response relationship.
Associated with vitamin A deficiency and with iron deficiency of the Plummer-Vincent syndrome.
Have orderly pattern of regional spread from mucosal site of origin and metastasizing to regional cervical lymph nodes.
79% of patients present with local or regional advanced disease and the treated with combined modality therapy.
More than half of the patients who present with locoregional advanced disease will recur within three years after treatment.
Approximately 16% of patients diagnosed with metastatic disease at presentation.
Incidence of base of tongue and tonsil cancers have increased, especially in individuals younger than 45 years.
Increased incidence in base of tongue and tonsil caners attributed to increased human papilloma virus infections associated with oral sex and increased number of sexual partners.
Patients with human papilloma associated cancers have a better prognosis, survival and cure rate than human papilloma virus negative squamous cell cancer.
HPV oropharynx cancers, tonsil and base of tongue, have a predilection for younger white males and seem to be molecularly different from tobacco related head and neck malignancies.
Smoking associated with decreased overall survival and progression free survival regardless of HPV16 status.
The incidence of cancers of the tonsil and tongue base associated with HPV has risen 5% per year in the US over the last few decades.
HPV related head and neck cancers are associated with less tobacco and alcohol exposure, less cardiopulmonary co-morbidity and their prognosis is better than tobacco associated head and neck cancers.
HPV positive disease in the lymphoid organ it is usually able to escape immune detection, including upregulation of PD-L, infiltration of tumor-infiltrating lymphocytes, and high expression of PD-L! receptor on T cell, all of which can promote adaptive resistance.
Five-year survival rates for locally advanced cancer 20-40%.
The majority are locoregionally advanced (stages III and IV) at the time of diagnosis.
Approximately 50 to 60% of patients with locally/regionally involved advanced head and neck cancer treated with radiation, surgery or both develop local regional recurrence in two years, and an additional 20 to 30% have developed distant metastases by that time.
The five year overall survival rate for squamous cell carcinoma of the head and neck is 40 to 50% in approximately 50% of patients with locally advanced squamous cell carcinoma of the head and neck experience recurrence after definitive therapy.
The median survival for patients with untreated metastatic or recurrent head and neck cancer is approximately 3 to 4 months.
Recurrent/metastatic head and neck squamous cell carcinoma (HNSCC) has a poor prognosis with a median overall survival (OS) of only 13 months in patients treated in the first-line setting and 6 months in previously treated patients.
Patients who have progression of their cancer within six months of receiving platinum-based chemotherapy have a median survival of six months or less.
Randomized trials comparing mono chemotherapy versus combination therapy have been unable to confirm superiority of any one versus another in metastatic or recurrent squamous cell carcinoma of the head and neck.
Surgery choice depends on tumor location, size, proximity to bone and depth of infiltration.
Radiation is typically delivered as daily fractions of 1.8 to 2 Gy to approximately 70 Gy over 6 to 7 weeks, with local control rates of 15 to 70% for local regional disease.
The management for localized disease Is usually single modality therapy with surgery or radiation.
Management of localized disease may include surgery followed by radiation.
About 80% of patients with local disease can be cured with the above management.
With regional disease patients receive multi modality therapy with curative intent, and they may undergo surgical resection, followed by radiation alone or in concurrence with chemotherapy.
For patients with locoregional disease the cure rate of only about 50% and is based on factors such as HPV status and comorbidities.
For patients with unresectable head and neck cancer the five-year survival rate with radiation alone is less than 25%.
Five year survival rate is 40%.
Metastatic squamous cell cancer associated with a median survival 6-9 months and 5 year survival less than 30%.
Patients with metastatic squamous cell disease that do not respond to first line treatment or experience recurrence have a median survival of 3-4 months.
Median survival for recurrent disease 10 months (Vermorken JB).
Distant metastases on presentation is relatively uncommon (less than 10%) but one third will develop distant disease.
For patients with advanced or relapsed squamous cell cancer of the head and neck the process is almost always fatal.
Autopsy studies have shown that the overall incidence of distant metastases is relatively high at 40-47%.
A significant number of patients suffer with functional and aesthetic complications of definitive treatment.
25-50% of patients present with marked nutritional impairment.
30-50% of patients lose 10% of body weight before they begin radiation therapy.
38.5% of patients that undergo radiation experience long-term dysphagia (Caudell)
Dysphagia almost nine times as prevalent in patients who undergo chemotherapy and concurrent radiotherapy as compared to radiation alone (Caudell).
Acute toxicity from concurrent chemoradiotherpay is markedly higher than in patients receiving sequential therapy, with grade 3 or 4 mucositis 43% vs 24% (Forastiere AA et al).
Concurrent chemotherapy and radiation therapy for head and neck cancer associated with higher incidence of grade three or four late toxicities, and the most common type of late toxicity is pharyngeal dysfunction.
Late toxicities of concurrent chemotherapy and radiation for head and neck cancer include feeding tube dependence, laryngeal dysfunction, and death, 13%, 12% and 10%, respectively (Machtay M et But al).
Efforts to prevent long-term dysphagia include utilizing swallowing exercises, and avoiding periods of nothing by mouth.
The incidence of postoperative infections in nutritional impaired patients may be as high as 20-50%.
Full mouth dental extractions frequently required in individuals with poor dentition.
About half patients have zinc deficiency.
Nutritional support 7-10 days before surgery decreases postoperative complications by 10%.
Up to 34% of patients undergoing chemotherapy and radiation experience severe dysphagia, 43% with moderate dysphagia and 22% have mild dysphagia: up to one third of such patients require artificial means of nutrition to maintain caloric intake.
Frequently 10% or greater weight loss during treatment with chemoradiation.
Severe mucositis develops in almost two thirds of patients treated with chemoradiation and a significant number require gastric feedings.
About 5% of cancers diagnosed annually.
Emotional and physical stress on patients with head neck cancer through diagnosis, treatment and surveillance is immense and greater than that experienced by other cancer survivors.
Rates of suicidality are twice that of other patients with cancer and triple that of the US general population
Median survival with metastases or recurrent cancer is only 6 months with conventional chemotherapy.
Oral cancer is the most common neoplasm of the head and neck with a worldwide incidence of 300,000 new cases annually.
Women comprise between 5 and 31% of head and neck patients.
2-year survival rate of adequately nourished patients with the undernourished patients is 57.5% vs. 7.5%.
Majority of patients have increased levels of EGFR expression.
EGFR and its principal ligand transforming growth factor alpha (TGFA) linked to poor outcome.
EGFR expression linked to resistance to chemotherapy and radiation therapy, worse disease free and overall survival.
EGFR inhibitors may synergize effects of chemotherapy and other anticancer treatments.
Majority of lesions overexpress VEGF2 or VEGF3. and such expressionis associated with decreased survival (Riedel F, Kyzas PA).
Radiologic imaging should be performed before large biopsy specimens are obtained, to avoid possible biopsy-induced anatomical distortion or biopsy-induced false positive results on positron- emission tomography.
Fine-needle aspiration biopsy is highly sensitive, specific, and accurate for the initial histologic diagnosis.
Cervical- node biopsy is required, complete nodal resection is preferable to prevent extracapsular metastatic spread and tumor spillage.
Chemotherapy delivery and the introduction of concurrent radiosensitizing systemic therapy and definitive radiotherapy have improved survival among patients with head and neck cancer and especially those with HPV-associated oropharyngeal cancer.
Phase II treatment of recurrent or metastatic disease with erlotinib, cisplatin and docetaxel resulted in a 48% overall response rate (Kim).
Cetuximab in addition to platinum based chemotherapy in platinum resistant patients with refractory or recurrent disease had a 10% response rate and a 53% tumor growth control rate (Baselga).
Combination of cisplatin and cetuximab results in a 20% response rate in patients who failed first line cisplatin and 18% of patients with previously stable disease (Herbst).
A clinical trial of patients with human papillomavirus (HPV)-positive oropharyngeal cancer demonstrated worse overall survival with cetuximab plus radiation therapy than with cisplatin plus radiation, the current standard treatment (NCI).
In patients with locally advanced head and nech cancer the addition of cetuximab to chemoradiation in a cooperative group trial showed no increased survival benefit with a 2 year progression free survival of 63.4% with cetuximab versus 64.3% with cisplatin-based chemoradiation alone (KK Ang et al).
In the EXTREME trial of patients with recurrent or metastatic disease receiving platinum based therapies and fluoracil only or the same drugs plus cetuximab: the addition of cetuximab significantly increased the median progression free trial 5.6 months vs 3.3 months and median survival 10.1 vs 7.4 months, respectively.
When two or more regional lymph nodes are involved or mucosal margins of resection are positive there are high rates of local recurrence (27-61%), distant metastases (18-21%) and low 5-year survival rates (27-34%).
Randomized trials have shown that the addition of chemotherapy to the curative treatment of patients with advanced head and neck cancer improves organ preservation rates, longer time to progression, improved locoregional control, fewer distant metastases and longer overall survival rates.
For patients with resectable locally advanced squamous cell cancer post operative concurrent administration of high dose cisplatin with radiotherapy is more efficacious than radiotherapy alone.
Cisplatin and 5FU followed by radiotherapy superior to radiotherapy alone and recent data suggest superiority of induction therapy with a taxane, platinum and 5FU is superior to 5FU plus cisplatin.
In a phase 3 study of 504 patient’s comparing docetaxel, cis-platinum and 5-FU compared to cis-platinum plus 5-FU, revealed 52% of the TPF patients were alive at 5 years.
Compared to TPF the PF regimen median survival was 71 months versus 35 months (TAX 324 Trial).
In the TAX trial laryngeal and hypopharyngeal primary tumors treated with the TPF regimen resulted in a 50% reduction in risk progression or death compared with PF.
Taxotere, platinum 5FU regimen (TPF) is presently the standard of care for inducton therapy for locally advanced head and neck cancer (2010).
In a meta-analysis of data from 10,741 patients enrolled in 63 randomized trials comparing locoregional treatment plus chemotherapy demonstrated the addition of concurrent chemotherapy to radiotherapy conferred and 8% higher survival rate at five years, compared with locoregional treatment alone (Pignon JP et al).
An update of the above meta-analysis confirmed survival benefit with concurrent chemo radiotherapy, with an absolute survival advantage of 6.5% at five years over at locoregional treatment alone (Pignon JP et al).
An analysis of 15 studies using platinum and 5FU induction chemotherapy has confirmed a significant survival advantage of 5% at five years, compared with local regional treatment alone, while this was not seen in the original meta-analysis (Monnerat C et al).
Weight of evidence support concurrent chemoradiation over neoadjuvant chemotherapy followed by surgery or radiation.
Most trials of neoadjuvant chemotherapy have not shown survival benefit over radiation alone.
In early stage lesions, or in patients with non-bulky primary tumors and or small volume lymphadenopathy locoregional control with radiation therapy alone can be excellent , and whether the addition of chemotherapy is beneficial is debatable.
Following resection in locally advanced squamous cell cancer concurrent chemoradiated patients have a 5-year estimate of progression-free survival of 47% compared to the radiation only group of 36%.
5-year rate of death in patients with locally advanced cancer and treated with resection and postoperative adjuvant chemoradiation was reduced from 43% to 27%.
Radiation therapy with cisplatin based chemotherapy presently standard of care in selected patients with nasopharyngeal, laryngeal, unresectable lesions and in the postoperative adjuvant setting.
Combined postoperative chemoradiation after resection of locally advanced cancer does not reduce the risk of distant metastases.
The addition of bevacizumab to platin based therapy in metastatic disease does not improve overall survival, but does improve progression free survival.
Development of intensity modulated radiation therapy spares adjacent dose limiting normal tissue damage to brain stem, optic nerves, spinal cord and salivary glands.
Radiotherapy can potentially cure any local stage or site lesion, but is best known for treating advanced disease with the intent of sparing removal of critical structures.
The 2 year progression free survival of patients receiving panitumumab plus radiation was not superior to patients receiving cisplatinum plus radiation (Siu LL).
1%-6% present with neck metastases and unknown primary.
Elective treatment of the neck is performed when the probability of metastases from some primary tumor of the head and neck is greater than 20%.
Elective radiotherapy of the neck has good results when the primary tumor is controlled.
Hypothyroidism occurs in the third to nearly half of patients who have received radiation to the neck, often as a late sequela.
More than 70% of clinical positive nodes subsequently have pathological disease.
Patients who have progressive disease after first line treatment or who have platinum refractory disease have a survival measured in weeks.
Combination chemotherapy regimens generally are associated with a 30-40% response rates with recurrent cancer but provides no improvement in overall survival compared to single agent regimens.
Platinum based systemic chemotherapy with EGFR inhibitor cetuximab results in a median overall survival of 10 months and is standard of care for fit patients with metastatic disease.
Docetaxel response rates of 27-43% in recurrent and metastatic lesions.
A study of 501 patients with stage III or IV nonmetastatic disease randomized to receive cisplatin and fluorouracil vs cisplatin, fluorouracil and docetaxel followed by carboplatin and radiation and in those eligible surgery: at 3 years overall survival was 48% for standard chemotherapy and 62% for the three agent treatment with median survival of 30 months vs 71 months, respectively (Posner).
Head and neck cancer-cisplatin, fluorouracil and docetaxel in the above study resulted in a 30% reduction in mortality.
Patients with pathologically proven extracapsular nodal disease or more than one node involvement are traditionally treated with postoperative radiation.
The anti-PD-1 antibody pembrolizumab produced broad and durable responses in patients with recurrent/metastatic head and neck squamous cell carcinoma (HNSCC).
Pembrolizumab has an overall response rate (ORR) of 25%, and it proved active in both HPV-positive and HPV-negative patients.
First-line therapy options for head and neck cancer should now include immunotherapy with pembrolizumab given alone or in combination with chemotherapy (CT), as indicated by the results of the KEYNOTE-48 trial.
The data support pembrolizumab plus platinum-based CT and pembrolizumab monotherapy as new first-line standard-of-care therapies for relapsed/metastatic head and neck squamous cell carcinoma.
KEYNOTE-48 was a randomized, open-label study that enrolled 882 patients with recurrent/metastatic HNSCC, which was incurable with local therapies.
Nivolumab in a phase III trial of patients refractory to platinum treatment there was a 30% reduction in risk of death compared to other treatments, and 1 year survival double to 36% vs 16% for controls.
Nivolumab prolongs survival in patients with recurrent or metastatic squamous cell carcinoma of the head and neck that has progressed after platinum-based chemotherapy compared with those who received standard single agent systemic chemotherapy.
At 3 years nivolumab monotherapy or nivolumab plus ipilumumab survival was 52% and 58%, respectively compared with ipilumab alone at 34% for metastatic H and N carcinoma.
Pembrolizumab seems to be roughly twice as effective, when measured by response as cetuximab in head and neck cancer.
KEYNOTE-012 study pembrolizumab administered at 10 mg/kg every 2 weeks, had a 20% response rate in patients with advanced HNSCC whose tumors were PD-L1-positive.
Keynote-012 and Keynote-055 demonstrated in refractory patients with metastatic disease, a response rate of 17%, with durable responses, with about half of the complete responses occurring after 6 months of therapy.
CheckMate 141 study with nivolumab had similar responses in metastatic disease to pembrolizumab, but for the first time showed an overall survival benefit compared to chemotherapy in a refractory population.
Atezolizumab did not improve clinical outcomes and patients with locally advanced squamous cell carcinoma of the head and neck at high risk of disease progression after multimodal definitive treatment (Haddad R).
Sentinel lymph node biopsy can be achieved for the majority of oral cavity and oropharyngeal tumors with an identification of 93% and a sensitivity of 93% at a mean follow-up of 24 months.
Sentinel lymph node biopsy most appropriate for stage I/II disease.
Sentinel lymph node biopsy emerging as the standard approach to staging patients with clinically node negative disease.
The American Joint Committee on Cancer (AJCC) uses the TNM (tumor, node, metastasis) staging system, along with the Union for International Cancer Control (UICC) system, to stage dis- ease and determine therapy for head and neck squamous-cell cancer.
Staging of head and neck cancer differs at each anatomical site.
Generally, early stages (I and II) involve smaller tumors without prominent lymph- node involvement.
Later stages (III and IV) are characterized by locally advanced disease and invasion of surrounding structures or an in- creased number of involved lymph nodes, with distant metastatic spread also defining stage IV.
Oropharyngeal cancer staging requires knowledge about HPV status.
Patients with HPV-associated (p16-positive) oropharyngeal cancer were younger, were more likely to be white, and had fewer smoking pack-years, smaller primary tumors, and significantly better outcomes than patients with HPV-negative disease, as well as a higher 8-year overall survival rate 70.9% vs. 30.2%.
5-year overall survival rates for HPV-positive oropharyngeal cancer were similar for stages I, II, III, and IVA but were significantly lower for stage IVB.
Survival does not differ significantly between patients with T4a tumors and those with T4b tumors, and survival does not differ significantly among patients with N0; N1, N2, or N2a; or N2b nodal subsets.
Survival is reduced among patients with N3 nodal disease.
The association between the results of p16 testing and survival is similar to the association between the results of other HPV detection methods and survival.
There is a good diagnostic concordance of 81.5% between p16 immunohistochemical testing and whole-exome sequencing for HPV-associated disease in the oropharynx.
Patients with HPV-associated (p16-positive) oropharyngeal cancer were younger, were more likely to be white, and had fewer smoking pack-years, smaller primary tumors, and significantly better outcomes than patients with HPV-negative disease, as well as a higher 8-year overall survival rate 70.9% vs. 30.2%.
5-year overall survival rates for HPV-positive oropharyngeal cancer were similar for stages I, II, III, and IVA but were significantly lower for stage IVB.
Survival does not differ significantly between patients with T4a tumors and those with T4b tumors, and survival does not differ significantly among patients with N0; N1, N2, or N2a; or N2b nodal subsets.
Survival is reduced among patients with N3 nodal disease. differs according to the stage of disease, anatomical site, and surgical accessibility.
For patients with HPV-positive oropharyngeal cancer showed that
patients with stage I disease who received definitive radiotherapy alone had reduced survival, as compared with patients undergoing chemoradiotherapy, surgery with adjuvant radiotherapy, or surgery with adjuvant chemoradiotherapy.
Patients with stage II disease who were treated with surgery alone or radiotherapy alone had poorer survival than those treated with chemoradiotherapy.
In HPV positive oropharyngeal cancer the five-year overall survival rates for stage is I, II, III, and IVA are similar but significantly lower with stage IVB.
5 year Survival rates are not different significantly between patients with T4a tumors in those with T4b tumors, and survival did not differ significantly among patients with N0, N1, N2, orN2b nodal subsets with HPV positive oropharyngeal cancer.
Patients with stage III disease who received chemo- radiotherapy alone had worse survival than those treated with upfront surgery followed by chemo- radiotherapy.
Since patients with locally advanced HPV-positive oropharyngeal carcinoma have long-term survival rates as high as 80%, morbidity and quality of life are major concerns.
Upfront surgery may allow for a reduc- tion in the total radiotherapy.
In patients with locally advanced oropharyngeal cancer and a high pre- dominance of HPV-positive status (>90%) have shown that robotic surgery and trans- oral laser microsurgery are feasible and allow adequate visualization with good functional re- sults and survival.
Approximately 30 to 40% of patients present with stage I or II disease.
Stage I and Ii disease are curable with surgery alone or definitive radiotherapy alone. long- term survival rates in approximately 70 to 90% of patients with early-stage disease.
The choice of treatment depends on anatomical accessibility, with efforts to minimize morbidity and preserve function.
Robotic surgery for oropharyngeal cancer and minimally invasive laser microsurgery for laryngeal and hypopharyngeal cancers may increase the likelihood of preserving function.
Advances in radiotherapy techniques such as intensity-modulated and image-guided radiotherapy may reduce morbidity.
Oropharyngeal cancers may be managed primarily with surgery or radiotherapy,
Selective neck dissection, elective neck dissection with more extensive removal of nodes, or pro- phylactic neck radiotherapy decreases the risk of recurrence and spread to ipsilateral or bilateral nodal sites, with treatment tailored to the site of the primary cancer.
More than 60% of patients with squamous-cell cancer of the head and neck present with stage III or IV disease.
Lymph nodes in the neck have historically been divided into anatomical
levels for the purpose of staging head and neck cancer and planning therapy.
The presence and sites of nodal metastases can greatly affect the treatment and prognosis.
Locally advanced disease carries a high risk of local reoccurrence of 15 to 40%.
Locally advanced disease carries a high risk of distant metastasis, with a poor prognosis-5-year overall survival, <50%.
Decisions about therapy depend strongly on the size and anatomical site of the primary cancer, stage of disease, age of the patient, patient preferences, performance status, and coexisting conditions.
Surgical resection is preferred for cancer of the oral cavity, in conjunction with elective neck dissection, followed by adjuvant radiotherapy or chemoradiotherapy.
Surgery is considered in patients with resectable tumors who have poor responses after induction chemotherapy, for persistent or recurrent disease in either the primary site or the regional lymph nodes after definitive chemoradiotherapy.
When surgical resection is less feasible or would result in poor long-term func- tional outcomes, chemoradiotherapy is the standard of care.
In a study involving 19,248 patients with resect-able or unresectable, locally advanced squamous- cell carcinoma of the head and neck, confirmed that the addition of concomitant chemotherapy with radiotherapy showed an absolute decrease in 5-year mortality of 6.5 percentage points and decreased loco-regional failure rates with chemoradiotherapy as compared with local therapy alone.
The addition of induction or adjuvant chemotherapy did not significantly im- prove overall survival, as compared with local therapy alone.
The RTOG 91-11 trial established
concurrent chemoradiotherapy for locoregional control and organ preservation in patients with resectable stage III or IV glottic or supraglottic disease.
Improved survival when chemotherapy was added to locoregional therapy.
Chemoradiotherapy is preferred for patients with good performance status who have advanced laryngeal or hypopharyngeal cancer without car- tilage involvement, whereas salvage laryngectomy is reserved for patients with recurrent or persistent disease or severe functional impairment.
Oropharyngeal cancer surgery for T3 or T4 tumors commonly includes prophylactic selective neck dissection or more extensive elective neck dissection, given the high rates of occult metastases.
Chemoradiotherapy provides excellent locoregional control of more advanced primary tumors.
High-dose cisplatin (100 mg per square meter of body-surface area, administered intravenously every 21 days for three cycles), given concur- rently with radiotherapy as part of a definitive chemoradiotherapy regimen, is the standard of care, with established survival benefits for patients with good performance status.
Carboplatin is commonly substituted for cisplatin in patients with coexisting renal impairment.
Carboplatin is less effective than high-dose cisplatin for definitive therapy.
The epidermal growth factor receptor antibody cetuximab, administered con- currently with radiotherapy, was an approved standard therapy on the basis of data showing that this regimen provided improvements in locoregional control and overall survival, as compared with radiotherapy alone.
Radiotherapy alone is no longer stan- dard care: recent randomized trials have shown worse outcomes, including decreased survival, with concurrent cetuximab and radio-
therapy in patients with HPV-positive oropharyngeal cancer, in a direct comparison with high- dose cisplatin combined with radiotherapy.
Data on the use of induction chemotherapy followed by chemoradiotherapy are conflicting and remain controversial.
Meta-analyses data support taxane-based induction regimens, showing that such regimens significantly decrease locoregional relapse and death rates, as compared with non– taxane-based regimens.
Induction chemotherapy is reserved for patients who are at high risk for locoregional relapse and distant metastases, patients for whom induction chemotherapy is likely to be associated with acceptable adverse event rates, or patients in whom symptomatic, locally advanced disease prevents adequate delivery of up-front curative chemoradiotherapy.
Trials established adjuvant chemoradiotherapy with high-dose cisplatin and conventional fractionation radiotherapy (60 to 66 Gy) as the standard of care in high-risk patients with squamous-cell carcinoma of the head and neck.
High-risk patients as those with T3 or T4 disease, positive surgical margins, extranodal spread, perineural or lymphovascular invasion, or vascular tumor embolism, or those with oral-cavity or oropharyngeal tumors with level IV or V nodes.
Chemoradiotherapy improved progression-free survival, locoregional control, and overall survival, as compared with radiotherapy alone, among these high-risk patients.
A median of 46 months of follow-up showed that chemoradiotherapy improved locoregional control and disease-free survival but not overall survival, as compared with radiotherapy alone, among these high-risk patients.
however, these improvements were no longer evident at a median follow-up of 9.4 years.
Studies supports the consensus that chemoradiotherapy benefits only patients with extranodal extension or positive surgical margins.
Recurrent or metastatic disease, or both, develops in more than 65% of patients with squamous- cell cancer of the head and neck.
Locally recurrent disease that cannot be treated with salvage surgery, radiotherapy, or a combination of the two has a dismal prognosis, which is similar to the prognosis with distant disease.
Such disease has a prognosis of 6 to 9 months in the absence of treatment.
Systemic therapy is the mainstay of palliation.
The phase 3 EXTREME (Erbitux in First-Line Treat- ment of Recurrent or Metastatic Head and Neck Cancer) trial established first-line standard-of- care therapy by showing that cetuximab added to chemotherapy consisting of
fluorouracil plus a platinum(cisplatinorcarboplatin),as compared with chemotherapy alone, significantly improved overall survival (10.1 months vs. 7.4 months), progression-free survival (5.6 months vs. 3.3 months), and the overall response rate (36% vs. 20%).
Erbitux, was less favorable because of the need for weekly administration of cetuximab which resulted in infusion reactions and skin reactions, and a poorer quality of life.
The anti–PD-1 antibodies pembrolizumab and nivolumab showed durable responses and survival improvements in platinum-treated pa- tients with recurrent or metastatic head and neck cancer
PD-1–directed immune-check- point inhibitor therapy can provide durable disease remission, improved survival, or both, but an estimated 85 to 95% of pa- tients with recurrent or metastatic head and neck cancer have no response to this treatment or have a response that is followed by disease progression and, ultimately, death from the disease.
Antineoplastic drugs with activity for squamous lesions include cisplatin, methotrexate, bleomycin, 5 FU, and etoposide.
Sunitinb trial in patients with recurrent or metastatic squamous cell carcinoma of the head and neck demonstrated modest activity, but may be associated with bleeding, worsening tumor skin ulceration or tumor fistula formation (Machiels J_P).
Definition of unresectable disease includes fixation of the primary site or lymphadenopathy to the spine or prevertebral muscles or involvement of the skin-base of skull, dura or brachial plexus.
Individuals may be categorized as unresectable, if a poor functional outcome following surgery or significant medical comorbidity exists.
Anemia as a result of concurrent chemoradiation may be seen in up to 80% of patients, with 17-28% having a hemoglobin less than eight g/dL.
Promising Activity With Palbociclib/Cetuximab in HNSCC Resistant to Platinum, Cetuximab
In a recent study of patients with platinum- or cetuximab-resistant, human papillomavirus (HPV)-unrelated head and neck squamous-cell carcinomas (HNSCC), promising activity was seen with palbociclib and cetuximab therapy.
HNSCCs are primarily driven by p16INK4A inactivation and cyclin D1 overexpression that leads to hyperactivation of CDK4/6.
EGFR inhibitor resistance is also caused by deregulated cyclin D1 expression.
62 patients with measurable, HPV-unrelated, recurrent or metastatic HNSCC.
All patients in the study were given palbociclib 125 mg daily on days 1 through 21 and cetuximab 400 mg/m2 on cycle 1, day 1, followed by 250 mg/m2 once weekly in cycles spanning 28 days.
Neutropenia was the most frequently reported grade 3-4 adverse event related to palbociclib, occurring in 21 (34%) patients overall. There were no treatment-related deaths documented.
In patients with platinum-resistant or cetuximab-resistant HPV-unrelated HNSCC, palbociclib and cetuximab results in promising activity outcomes.