 A precancerous lesion that can be effectively treated to prevent invasive cervical cancer.
A precancerous lesion that can be effectively treated to prevent invasive cervical cancer.
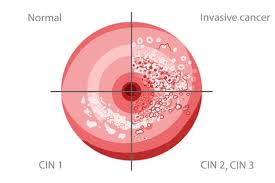
Graded by proportional thickness of abnormal cells with grades ranging from 1 to 3.
Cervical infections termed cervical intraepithelial neoplasia (CIN) 1,2,3 , signify neoplasia being present through the lower 1/3(CIN 1) 2/3 (CIN2 ), or the complete thickness of the epithelium(CIN3).
Cancer prevention achieved by removing CIN grades 2 and 3, i.e. high grade dysplasia, with excision (cone biopsy, loop excision,) or destruction (laser, cryotherapy) of such cells.
Colposcopic biopsy results are reported using for Bethesda system as CIN1,2.3 or squamous terminologies LSIL or HSIL.
LSIL approximately corresponds to CIN1 and histologic HSIL to CIN2 and CIN3.
50 to 60% of CIN2 lesions will regress and these patients can be monitored by frequent surveillance with repeated coloscopy or excisional treatment.
CIN3 is more likely to correlate with cellular transformation and risk for progression to cancer who is associated with highly questionable carcinogenic HPV genotypes.
Treatment is recommended for all non-pregnant individuals with a diagnosis of CIN3, or histological HSIL
Standard treatment has shifted from cold-knife conization toward less radical therapies.
Loop electrosurgical excision procedure widely used for treatment.
WHO guidelines for treatment of CIN grade 2 or 3 recommend either cryotherapy or loop electro surgical excision procedure (LEEP).
Conservative treatment reduces the risk of appearance of cervical cancer but they still are more likely to develop invasive cancer than the general population.
Common treatment of CIN of all grades carries a risk of persistence of 3-5% and a risk of recurrence of 13-19%.
Cervical intraepithelial neoplasia grade 2-3 occurs in 5-14% of women, and among women with HIV recurrence rate are as high as 27%.
1/3 of cervical intraepithelial neoplasia grade 2 or 3 can progress to invasive cancer, therefore these lesions must be removed or destroyed.
Treatment of pre-cancer involves excision of the destruction of the entire squamocolumnar junction in addition to the structure of lesions detected on colposcopy.
Treatment aims to eliminate the majority of HPV infected cells that have undergone pre-cancerous transformation to reduce the risk of developing a cervical cancer.
Most excisional treatments are performed using electrocautery such as loop electrical excision procedure or large loop excision of the transformation zone, although cold knife cone can be used.
Excisional procedures are preferred but ablation therapies are acceptable.
Ablation techniques include cryotherapy and thermal ablation.
10% of patients who had a high-grade squamous intraepithelial lesion (HGSIL, which includes so-called moderate-to-severe dysplasia, carcinoma in situ [CIS], and cervical intraepithelial neoplasia [CIN] II and III) will have persistent lesions that eventually would progress to invasive cancer without treatment.
The most common treatment modality is excisional biopsy: large loop excision of the transformation Zone or Loop electrosurgical excision procedure, laser conization, or cold knife conization.
The significant advantage of excisional compared with ablation of treatments is the ability to examine the abnormal excised specimen for pathological review, confirming the diagnosis, excluding an occult malignancy, and obtaining information about the completeness of excision.
The failure rate of excisional management, defined as persistent or recurrent CIN of grade 2 or worse is between 4 and 18%, and the majority of these cases occur within two years after primary treatment.
