 Anatomic description of site of fracture usually the proximal, middle or distal bone, also epiphyseal, metaphyseal and diaphyseal described as the head, base, and shaft, respectively.
Anatomic description of site of fracture usually the proximal, middle or distal bone, also epiphyseal, metaphyseal and diaphyseal described as the head, base, and shaft, respectively.
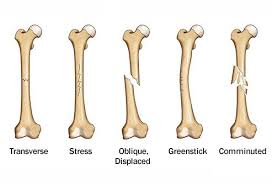
A transverse fracture describes a fracture that runs relatively perpendicular to the long axis of the bone, an oblique fracture describes one that is angled, a spiral fracture goes around and along a long bone.
Comminuted fractures have more than 2 fragments.
Intraarticular fractures involve the joint surface.
Alignment refers to the distal fragment relative to the proximal fragment and includes angular deformity in coronal or sagittal plane, rotation deformity around the long axis of the bone, translation refers to an angular coronal or sagittal displacement with decreased bone apposition, and shortening of the bone due to loss of bone length through the fracture.
Stable fractures refer to those that are not likely to displace after reduction and immobilization.
Unstable fractures refer to those lesions which are unable to be reduced or are likely to separate after immobilization.
Open or compound fractures refer to those cases with disruption of skin and tissues so that the fracture communicates with the external environment.
Closed fractures are those that do no communicate with the external environment.
Treatment includes the initial reduction, if indicated, and then immobilization.
Immobilization prevents further injury t soft tissues and is usually needed for fracture healing.
Nondisplaced fractures and those that can be adequately reduced in a closed fashion and have sufficient stability to heal adequately usually do not require surgery.
Fractures not able to be reduced in a closed fashion and those that are too unstable to maintain reduction or have significant joint involvement are usually treated surgically with open reduction and internal fixation, intramedullary nailing, external fixation or joint arthroplasty.
Certain stable fractures such as hip fractures are treated with surgery to prevent morbidity associated with prolonged immobility needed with nonoperative treatment.
Physeal plate injuries are common injuries in children since they are the weakest part of bone.
Pediatric fractures differ from adult fractures in that they have stronger more vascular periosteum leading to nondisplaced fractures that heal rapidly due to the strength of the periosteum.
Bones in the pediatric population are softer and more pliable than in the adult population and frequently there can be incomplete fractures.
Salter-Harris classification categorizes plate fractures into five types based on severity and likelihood of growth impairments.
Salter-Harris classification: Type I fracture through a growth plate without metaphyseal or epiphyseal involvement. Type II injury involves a fracture through the growth plate with a metaphyseal fracture, Type III fracture is a fracture through the growth plate with involvement of an epiphyseal fracture, Type IV fracture involves the growth plate the metaphysis and exits at the epiphysis, and Type V fracture is an severe crush injury to the growth plate.
More common than heart disease or cancer in women, affecting 1 in 2 women and 1 in 6 men older than 50 years.
Cancer can adversely affect the skeleton leading to decreases in bone mineral density, osteoporosis, and non-metastatic fractures.
Cancer treatments with glucocorticoids, hormone deprivation therapy, immunomodulatory therapy, surgical treatment, such as gastrectomy and hysterectomy with bilateral salpingohysterectomy, and radiation therapy can increase fracture risk.
Meta-analyses indicate an approximate 2 fold relative risk for subsequent fracture and 4 fold increased risk for those with a vertebral fracture and a subsequent vertebral fracture in women, with similar but less clear percentages for men.
Internal fixation with intramedullary nails and plate and screw combinations allow the surgeon to align and stabilize the bone.
Patients must be observed for the development of compartment syndrome, particularly with forearm or leg fractures.
Possibility of neurovascular injuries can occur with plaster immobilization and secondary swelling.
Unlike other tissues heal with normal histological findings without fibrous scar.
Subsequent risk of fracture greatest soon after a fracture, particularly in the first year.
Four months after a fragility fracture 85% of patients are still taking one or more drugs known to increase fracture risk (Munson J).
While rationale for high lifelong milk consumption is to meet calcium requirements for bone health, countries with the highest intakes of milk and calcium tend to have the highest rates of hip fractures.
Older people who had broken bones closer to the center of the body such as proximal fractures, such as upper arm or leg, pelvis, and ribs, had a greater risk of being admitted to the hospital for major medical conditions.
Such patients also faced a greater risk of dying prematurely following their fracture compared to similarly aged patients without fractures.
Proximal fractures included hip; femur; pelvis; rib; clavicle; and humerus and had increased mortality compared to those without fractures.
Mortality risk in the elderly at 2 years follow-up was increased for proximal fractures regardless of whether they were admitted to the hospital after the injury.
Those with distal fractures ( ankle, wrist) had similar or lower death risk and similar admission patterns as patients without fractures.
Among patients with closed extremity fractures, skin antisepsis with iodine povacrylex in alcohol resulted in fewer surgical site infections, than antisepsis with chlorhexidine gluconate in alcohol.
