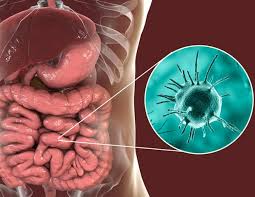
 Parasitic disease.
Parasitic disease.
Organism Entamoeba histolytica causes estimated 50 million infections and more than 100,000 deaths worldwide each year.
Most patients are infected asymptomatic cyst carriers, but a few patients may have a progressive clinical course.
Bulk of infected patients harbor E dispar which is 10 times more prevalent than E histolytica, with E dispar being nonpathogenic and E histolytica being pathogenic but mostly asymptomatic.
Also known amebic dysentery.
An infection caused by any of the amebae of the Entamoeba group.
Symptoms are most common during infection by Entamoeba histolytica.
Infection is more common in warmer areas: due to poorer hygiene and the parasitic cysts surviving longer in warm moist conditions.
Most infections are now believed due to E. dispar.
E. dispar is more common in certain areas and symptomatic cases may be less common than previously reported.
Patients present with no, mild, or severe symptoms.
Most infected people, about 90%, are asymptomatic.
Symptoms may include: abdominal pain, diarrhea, or bloody diarrhea.
Complications can include: colitis, ulceration of the colon with tissue death or perforation.
It is estimated that about 40,000 to 100,000 people worldwide die annually due to amoebiasis.
It may result in peritonitis.
Chronic iron deficiency may occur.
It is present all over the world, but most cases occur in the developing world.
>480 million cases worldwide, with between 40,000–110,000 deaths a year.
Cysts of Entamoeba cysts can survive for up to a month in soil or for up to 45 minutes under fingernails.
Invasion of the intestinal lining by cysts results in bloody diarrhea.
The parasite can reach the bloodstream it can spread through the body.
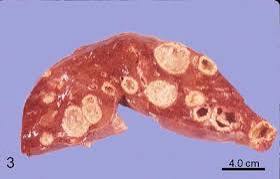
In the liver it can cause liver abscesses, which can occur without previous diarrhea.
Diagnosis is usually achieved by stool examination.
Leukocytosis may be present in severe cases.
The most accurate test is specific antibodies to amebiasis in the blood.
The positive antibody may remain positive following treatment.
No vaccine is available.
Attempts at prevention include: improved sanitation, including separating food and water from feces.
Amoebiasis in tissues is treated with either metronidazole, tinidazole, nitazoxanide, dehydroemetine or chloroquine.
Intestinal luminal infection is treated with diloxanide furoate or iodoquinoline.
Effective treatment may require a combination of drugs.
Infected patients without symptoms do not require treatment.
Infected individuals can spread the parasite to others and treatment should be considered.
In the absence of treatment the infections can last for years.
The ingestion of one viable cyst may cause an infection.
Symptoms take from a few days to a few weeks to develop, but usually it is about two to four weeks.
Symptoms can range from none to mild diarrhea to dysentery with blood, with intense abdominal pains.
The amoebae can invade the lining of the colon and cause bleeding.
In about 10% of invasive cases of amebiasis the amoebae enter the bloodstream and may travel to other organs, most commonly to the liver.
The average asymptomatic infection is estimated to persist for over a year.
The absence of symptoms or varied intensity is related to factors such as as strain of amoeba, immune response of the host, and perhaps associated bacteria and viruses.
In asymptomatic infections, the amoeba eat and digest bacteria and food particles in the gut, but do not usually come in contact with the intestine itself due to the protective layer of mucus that lines the gut.
When amoeba are able to contact GI mucosa they secrete enzymes that destroy cell membranes and proteins leading to penetration and digestion of tissues with formation of ulcerations in the intestine.
Entamoeba histolytica can ingest the destroyed cells by phagocytosis.
Steroid therapy can lead to severe amoebic colitis in persons with E. histolytica infection, with or without symptomatic disease.
Amoebic colitis is associated with high mortality, and on average more than 50% with severe colitis die.
Amoebiasis is usually transmitted by the fecal-oral route.
It can also be transmitted indirectly through contact with dirty hands or objects as well as by anal-oral contact.
Infection is spread through ingestion of the cyst form of the parasite.
The amoebae cyst is semi-dormant and hardy structural form found in feces.
Any non-encysted amoebae, or trophozoites, die quickly after leaving the body and are rarely the source of new infections.
Transmission through contaminated food and water, results in it beings endemic in regions of the world with limited modern sanitation.
E. histolytica causes tissue damage by three main events: direct host cell killing, inflammation, and parasite invasion.
Asymptomatic human infections are usually diagnosed by finding cysts released in the stool.
Cysts are shed intermittently and a minimum of three stools are examined.
With symptomatic Amebiasis, trophozites, the motile form of the parasite can often be seen in fresh feces.
Most infected individuals test positive for the presence of antibodies: Whether symptomatic or not.
The serum levels of antibody are much higher in individuals with liver abscesses.
Serological testing for amebiasis becomes positive about two weeks after infection.
Detecting ameba proteins and DNA in feces are available..
Microscopy is the most common method of diagnosis around the world, but it is not as sensitive or accurate in diagnosis as the other tests available.
As cysts are shed intermittently and may not show up in every sample, stool examination for cysts or trophozoites may require examination of several samples, over several days.
E. histolytica cysts have a maximum of four nuclei, can be distinguished from the commensal Entamoeba coli cyst which has up to 8 nuclei.
E. histolytica can be distinguished from Entamoeba coli by location of the endosome and shape of chromatoidal bodies.
However, microscopy cannot distinguish E. histolytica from other non-pathogenic amoebae.
Therefore, the WHO recommends not treating patients who are asymptomatic, based on microscopic diagnostic findings alone.
Once the disease goes extra-intestinal, the organism can no longer be found in the stool.
Serological tests are useful in detecting infection by E. histolytica if the organism goes extra-intestinal.
An Ova & Parasite (O&P) test or an E. histolytica fecal antigen assay is the proper assay for intestinal infections.
Antibodies may persist for years after cure, so that a positive serological result may not necessarily indicate an active infection.
A negative serological result, excludes a suspected tissue invasion by E. histolytica.
Stool antigen detection tests can overcome some of the limitations of stool microscopy.
Polymerase chain reaction (PCR) is considered the gold standard for diagnosis.
To help prevent infection:
Avoid raw vegetables in endemic areas, as they may have been fertilized using human feces.
Avoid eating street foods especially in public places.
Responsible sewage disposal or treatment.
Sedimentation and filtration of water supplies are necessary to reduce the incidence of infection, as E. histolytica cysts are usually resistant to chlorination.
E. histolytica infections occur in both the intestine and or liver.
Symptomatic patient required treatment with two agents: an amebecidal tissues active agents and a luminal cysticidal agent.
Overwhelmingly, ameobas remain in the G.I. tract.
Ulceration of the G.I. mucosal surfaces occurs in less than 16% of cases.
In a few cases there is invasion of soft tissues, most commonly the liver.
Complications of the infection includes intestinal obstruction, bloody diarrhea, pericolic and pericecal abscesses.
Complications of hepatic amoebiasis includes subdiaphragmatic abscess, perforation of diaphragm to pericardium and pleural cavity, amoebic peritonitis and perforation of skin.
The lungs can be involved from hepatic hematogenous spread of amoeba and also from perforation of the pleural cavity and lung.
Pulmonary amebiasis can cause lung abscess, pulmono pleural fistula, empyema lung and broncho pleural fistula.
Amoebas can reach the brain through hematogenous spread and cause brain abscess and amoebic meningoencephalitis.
Cutaneous amoebiasis can occur in skin around sites of involvement.
Urogenital tract amoebiasis can be caused by an intestinal lesion and can cause amoebic vulvovaginitis, rectovesicle fistula and rectovaginal fistula.
Amebiasis infection can be associated with malnutrition and stunting of growth.
There are approximately 50 million true E. histolytica infections and approximately seventy thousand die each year, mostly from liver abscesses or other complications.
In addition to E. hitolytics evidence shows there are at least two other species of Entamoeba that look the same in humans: E. moshkovskii and Entamoeba bangladeshi.
