Heart sounds are generated by the beating heart and the resultant flow of blood through it.
Heart sounds reflect the turbulence created when the heart valves snap shut.
In cardiac auscultation, the examiner uses a stethoscope to listen for these distinct sounds that provide important auditory data regarding the condition of the heart.
First heart sound: caused by atrioventricular valves – Mitral (M) and Tricuspid (T).
Second heart sound caused by semilunar valves – Aortic (A) and Pulmonary/Pulmonic (P).
In healthy adults, there are two normal heart sounds, often described as a lub and a dub that occur in sequence with each heartbeat.
These are the first heart sound (S1) and second heart sound (S2), produced by the closing of the atrioventricular valves and semilunar valves, respectively.
In addition to these normal sounds, other sounds may be present including heart murmurs, adventitious sounds, and gallop rhythms S3 and S4.
Heart murmurs are generated by turbulent flow of blood..
Heart murmur, to be heard as turbulent flow, must require pressure difference of at least 30 mm of Hg between the chambers.
The pressure dominant chamber will outflow the blood to non-dominant chamber in diseased condition which leads to Left-to-right shunt or right-to-left shunt based on the pressure dominance.
Turbulence outside the heart then the turbulence is called bruit or vascular murmur.
Murmurs may be physiological (benign) or pathological (abnormal).
Abnormal murmurs can be caused by stenosis that restricts the opening of a heart valve, resulting in turbulence as blood flows through it.
Abnormal murmurs may also occur with valvular insufficiency (regurgitation).
This allows backflow of blood when the incompetent valve closes with only partial effectiveness.
These murmurs are audible in different parts of the cardiac cycle, depending on the cause of the murmur.
Diagram showing relations of opened heart to front of thoracic wall.
Normal heart sounds are associated with heart valves closing.
First heart sound
The first heart sound, or S1, is composed of components M1 (mitral valve closure) and T1 (tricuspid valve closure).
Normally M1 precedes T1 slightly.
The first heart sound is caused by the closure of the atrioventricular valves, i.e. tricuspid and mitral (bicuspid), at the beginning of ventricular contraction, or systole.
When the ventricles begin to contract, so do the papillary muscles in each ventricle.
The papillary muscles are attached to the cusps or leaflets of the tricuspid and mitral valves via chordae tendineae.
When the papillary muscles contract, the chordae tendineae become tense and thereby prevent the backflow of blood into the lower pressure environment of the atria.
The chordae tendineae allow the leaflets of the valve to balloon up into the atria slightly, but not so much as to evert the cusp edges and allow backflow of blood.
The pressure created from ventricular contraction closes the valve, not the papillary muscles themselves.
The contraction of the ventricle begins just prior to AV valves closing and prior to the opening of the semilunar valves.
The sudden tensing of the chordae tendineae and the squeezing of the ventricles against closed semilunar valves, send blood rushing back toward the atria, and the parachute-like valves catch the rush of blood in their leaflets causing the valve to snap shut.
The S1 sound results from reverberation within the blood associated with the sudden block of flow reversal by the valves.
The delay of T1 even more than normally causes the split S1 which is heard in a right bundle branch block.
The second heart sound, or S2, is composed of components A2 (aortic valve closure) and P2 (pulmonary valve closure).
Normally A2 precedes P2 especially during inspiration where a split of S2 can be heard.
It is caused by the closure of the semilunar valves (the aortic valve and pulmonary valve) at the end of ventricular systole and the beginning of ventricular diastole.
As the left ventricle empties, its pressure falls below the pressure in the aorta.
Aortic blood flow quickly reverses back toward the left ventricle.
the blood is caught by the pocket-like cusps of the aortic valve, and is stopped by aortic valve closure.
As the pressure in the right ventricle falls below the pressure in the pulmonary artery, the pulmonary valve closes.
The S2 sound results from reverberation within the blood associated with the sudden block of flow reversal.
Splitting of S2, also known as physiological split, normally occurs during inhalation because the decrease in intrathoracic pressure increases the time needed for pulmonary pressure to exceed that of the right ventricular pressure.
A widely split S2 can be associated with several different cardiovascular conditions, and the split is sometimes wide and variable whereas, sometimes wide and fixed.
The wide and variable split occurs in right bundle branch block, pulmonary stenosis, pulmonary hypertension and ventricular septal defects.
The wide and fixed splitting of S2 occurs in atrial septal defect.
Pulmonary S2 (P2) will be accentuated (loud P2) in pulmonary hypertension and pulmonary embolism.
S2 becomes softer in aortic stenosis.
Extra heart sounds form gallop rhythms and are heard in both normal and abnormal situations.
The third heart sound, or S3 is rarely heard.
The third heart sound is also called a protodiastolic gallop, ventricular gallop, or informally the “Kentucky” gallop,an onomatopoeic reference to the rhythm and stress of S1 followed by S2 and S3 together (S1=Ken; S2=tuck; S3=y).
If new, a third heart sound indicates heart failure or volume overload.
The third heart sound occurs at the beginning of diastole after S2 and is lower in pitch than S1 or S2 as it is not of valvular origin.
The third heart sound is benign in the young, some trained athletes, and sometimes in pregnancy but if it re-emerges later in life it may signal cardiac problems, such as a failing left ventricle as in dilated congestive heart failure.
S3 is thought to be caused by the oscillation of blood back and forth between the walls of the ventricles initiated by blood rushing in from the atria.
The third heart sound does not occur until the middle third of diastole as during the early part of diastole, the ventricles are not filled sufficiently to create enough tension for reverberation.
It may also be a result of tensing of the chordae tendineae during rapid filling and expansion of the ventricle.
A S3 heart sound indicates increased volume of blood within the ventricle.
An S3 heart sound is best heard with the bell-side of the stethoscope which is used for lower frequency sounds.
A left-sided S3 is best heard in the left lateral decubitus position and at the apex of the heart, which is normally located in the 5th left intercostal space at the midclavicular line.
A right-sided S3 is best heard at the lower left sternal border.
A right-sided S3 will increase on inhalation, while a left-sided S3 will increase on exhalation.
S3 can be a normal finding in young patients but is generally pathologic over the age of 40.
The most common cause of pathologic S3 is congestive heart failure.
The fourth heart sound, or S4 when audible in an adult is called a presystolic gallop or atrial gallop.
This gallop is produced by the sound of blood being forced into a stiff or hypertrophic ventricle.
The fourth heart sound is a sign of a pathologic state, usually a failing or hypertrophic left ventricle, as in systemic hypertension, severe valvular aortic stenosis, and hypertrophic cardiomyopathy.
The sound occurs just after atrial contraction at the end of diastole and immediately before S1, producing a rhythm.
It is best heard at the cardiac apex with the patient in the left lateral decubitus position and holding their breath.
The combined presence of S3 and S4 is a quadruple gallop.
At rapid heart rates, S3 and S4 may merge to produce a summation gallop.
Atrial contraction must be present for production of an S4, and is absent in atrial fibrillation and in other rhythms in which atrial contraction does not precede ventricular contraction.
Heart murmurs are produced by turbulent flow of blood strong enough to produce audible noise.
The whooshing sound termed murmur only refers to a sound believed to originate within blood flow through or near the heart.
Rapid blood velocity is necessary to produce a murmur.
Most heart problems do not produce any murmur and most valve problems also do not produce an audible murmur.
Regurgitation through the mitral valve is by far the most commonly heard murmur, producing a pansystolic/holosystolic murmur which is sometimes fairly loud to a practiced ear, even though the volume of regurgitant blood flow may be quite small.
About 20% of cases of mitral regurgitation do not produce an audible murmur.
Stenosis of the aortic valve is typically the next most common heart murmur, a systolic ejection murmur.
Aortic stenosis is more common in older adults or in those individuals having a two-leaflet, not a three-leaflet, aortic valve.
Regurgitation through the aortic valve, if marked, is sometimes audible to a practiced ear. Generally, this is a very rarely heard murmur, even though aortic valve regurgitation is not so rare.
Aortic regurgitation, usually does not produce an audible murmur.
Stenosis of the mitral valve, if severe, also rarely produces an audible, low frequency soft rumbling murmur.
It is best recognized by a practiced ear using high quality, especially electronically amplified, stethoscope.
Grade Description Grade 1 Very faint, heard only after listener is listening intently, butmay not be heard in all positions.
The murmur may only be heard if the patient performs the Valsalva maneuver.
Grade 2 Quiet, but heard immediately after placing the stethoscope on the chest.
Grade 3 Moderately loud.
Grade 4 Loud, with palpable thrill.
Grade 5 Very loud, with thrill. May be heard when stethoscope is partly off the chest.
Grade 6 Very loud, with thrill.
May be heard with stethoscope entirely off the chest.
With the advent of better quality and wider availability of echocardiography and other techniques, heart status can be recognized and quantified much more accurately than formerly possible with only a stethoscope.
Inhalation decreases intrathoracic pressure which allows more venous blood to return to the right heart pulling blood into the right side of the heart via a vacuum-like effect.
Right-sided heart murmurs generally increase in intensity with inhalation.
The decreased intrathoracic pressure has an opposite effect on the left side of the heart, making it harder for the blood to exit into circulation.
Therefore, left-sided murmurs generally decrease in intensity during inhalation.
Increasing venous blood return to the right side of the heart by raising a patient’s legs to a 45-degree while lying supine produces similar effect which occurs during inhalation.
Inhalation can also produce a non-pathological split S2 which will be heard upon auscultation.
With exhalation, the opposite haemodynamic changes occur: left-sided murmurs generally increase in intensity with exhalation.
Interventions that can be performed that alter the intensity and characteristics of abnormal heart sounds.
These interventions can differentiate the different heart sounds to more effectively obtain a diagnosis of the cardiac anomaly that causes the heart sound.
Clicks – Heart clicks are short, high-pitched sounds that can be appreciated with non-invasive imaging techniques.
Rubs – The pericardial friction rub can be heard in pericarditis, an inflammation of the pericardium, the sac surrounding the heart.
It is a characteristic scratching, creaking, high-pitched sound emanating from the rubbing of both layers of inflamed pericardium.
The pericardial friction rub is loudest in systole, but can often be heard at the beginning and at the end of diastole.
The pericardial friction rub is very dependent on body position and breathing, and changes from hour to hour.
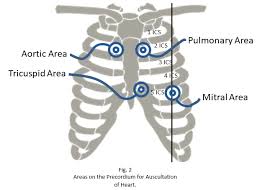
The aortic area, pulmonic area, tricuspid area and mitral area are areas on the surface of the chest where the heart is auscultated.
Heart sounds result from reverberation within the blood associated with the sudden block of flow reversal by the valves closing.
Auscultation to determine function of a valve is usually not performed at the position of the valve, but at the position to where the sound waves reverberate.
Aortic valve (to aorta) right second intercostal space upper right sternal border
Pulmonary valve (to pulmonary trunk) left second intercostal space upper left sternal border
Tricuspid valve (to right ventricle) left fourth, fifth intercostal spaces lower left sternal border
Mitral valve (to left ventricle) left fifth intercostal space left midclavicular line

 See heart murmurs
See heart murmurs