 Congenital diaphragmatic hernia (CDH) is a birth defect of the diaphragm.
Congenital diaphragmatic hernia (CDH) is a birth defect of the diaphragm.
The most common type of CDH is a Bochdalek hernia.
Other CDH types include Morgagni hernia, diaphragm eventration and central tendon defects of the diaphragm.
Hiatal hernia is a caused by the developmental abnormality in the esophageal hiatus and lead to herniation of the gastroesophageal junction, stomach or intestine through the esophageal hiatus.
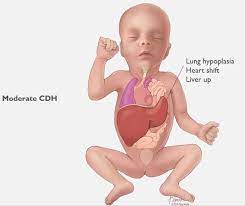
Malformation of the diaphragm allows the abdominal organs to push into the chest cavity, hindering proper lung formation and function.
CDH is a life-threatening pathology in infants.
It is a major cause of death due to two complications of pulmonary hypoplasia and pulmonary hypertension.
Newborns with CDH often suffer with severe respiratory distress which can be life-threatening unless treated appropriately.
The Bochdalek hernia, (postero-lateral diaphragmatic hernia) is the most common manifestation of CDH, accounting for more than 95% of cases.
The Bochdalek hernia is characterized by a hole in the postero-lateral corner of the diaphragm which allows passage of the abdominal viscera into the chest cavity.
The majority of Bochdalek hernias (80–85%) occur on the left side of the diaphragm.
Bochdalek hernias carry a high mortality and is an active area of clinical research.
A rare anterior defect of the diaphragm is variably referred to as a Morgagni hernia retrosternal, or parasternal hernia.
Morgagni hernia accounts for approximately 2% of all CDH cases, it is characterized by herniation through the foramina of Morgagni which are located immediately adjacent and posterior to the xiphoid process of the sternum.
Morgagni hernia are rarely identified on fetal ultrasound.
In between 34 and 50% of such hernias are associated with other congenital anomalies such as Down syndrome or AV septal defect.
Approximately 2/3 of patients with Moragagni hernia are symptomatic in infants or childhood and present with respiratory symptoms, such as recurrent chest infections or chronic cough, G.I. symptoms, such as gastric pain, and or nausea and vomiting, or a combination of pulmonary and gastrointestinal symptoms.
Congenital diaphragmatic eventration refers to an abnormal displacement of part or all of an otherwise intact diaphragm into the chest cavity.
This rare type of CDH occurs because in the region of eventration the diaphragm is thinner, allowing the abdominal viscera to protrude upwards.[citation needed]
Genetic causes of CDH including aneuploidy chromosome copy number variants, and single gene mutations.
Gene mutations including LONP1[6] and MYR associated with CDH, involving three major defects: A failure of the diaphragm to completely close during development Herniation of the abdominal contents into the chest Pulmonary hypoplasia
Infants born with diaphragmatic hernia experience respiratory failure due to both pulmonary hypertension and pulmonary hypoplasia.
Infants with CDH often present with respiratory distress after birth, and most of these infants have a Bochdalek hernia.
Among the 5 to 25% of children with CDH who have minimal or no symptoms in the neonatal period CDH may be detected in childhood or even adulthood.
There is a restriction of blood flow through the lungs thought to be caused by defects in the lung.
Pulmonary hypoplasia/decreased lung volume is directly related to the abdominal organs presence in the chest cavity which causes the lungs to be severely undersized, especially on the side of the hernia.
CDH outcome is largely dependent on the severity of the defect and the appropriate timing of treatment.
2/3 of all CDHs can be detected on routine fetal ultrasound with a mean gestational age of diagnosis of 22 to 24 weeks.
A small percentage of cases go unrecognized into adulthood.
The first step in management is orogastric tube placement and securing the airway by intubation, and placed on a ventilator.
Ideally, the baby will never take a breath, to avoid air going into the intestines and compressing the lungs and heart.
Extracorporeal membrane oxygenation (ECMO) has been used as part of the treatment strategy at some hospitals.
Diaphragm eventration is typically repaired thoracoscopically, by a plication of the diaphragm.
Plication basically involves a folding of the eventrated diaphragm.
Congenital diaphragmatic hernia has a mortality rate of 40–62%.
Outcomes being more favorable in the absence of other congenital abnormalities.
Individual rates vary greatly dependent upon multiple factors: size of hernia, organs involved, additional birth defects and/or genetic problems, amount of lung growth, age and size at birth, type of treatments, timing of treatments, complications and lack of lung function.
