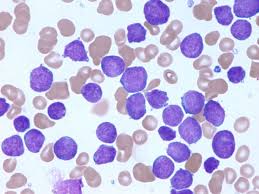
 Philadelphia chromosome-negative acute lymphoblastic leukemia (Ph-negative ALL) refers to a subtype of acute lymphoblastic leukemia (ALL) that does not exhibit the Philadelphia chromosome (Ph), which is characterized by the BCR-ABL1 fusion gene.
Philadelphia chromosome-negative acute lymphoblastic leukemia (Ph-negative ALL) refers to a subtype of acute lymphoblastic leukemia (ALL) that does not exhibit the Philadelphia chromosome (Ph), which is characterized by the BCR-ABL1 fusion gene.
It encompasses a variety of genetic and molecular abnormalities distinct from those seen in Philadelphia chromosome-positive (Ph-positive) ALL.
One subtype within Ph-negative ALL is Philadelphia chromosome-like (Ph-like) ALL, which shares a gene expression profile similar to Ph-positive ALL but lacks the BCR-ABL1 fusion gene.
Ph-like ALL is characterized by a range of genomic alterations that activate kinase and cytokine receptor signaling pathways, such as CRLF2 rearrangements and ABL-class fusions.
Ph-like ALL is associated with poor clinical outcomes, including high minimal residual disease (MRD) levels after induction therapy, high relapse rates, and inferior event-free and overall survival compared to other ALL subtypes.
The identification of Ph-like ALL is crucial for risk stratification and therapeutic decision-making.
Adolescents and young adults (AYAs) with Philadelphia chromosome–negative acute lymphoblastic leukemia (ALL) represent a unique patient population with a disproportionate survival disadvantage compared with younger children.
Improvements in survival have been achieved with the use of pediatric-inspired protocols in the front-line setting, as well as antibody-based and chimeric antigen receptor T-cell therapies in the relapsed and refractory setting.
The incorporation of minimal residual disease testing to inform clinical decision making represents major paradigm shifts in management.
AYA defined as an individual age 15 to 39 years of age at the time of cancer diagnosis.
There is a sharp decline in 5-year ALL survival rates from 75% at age 17 years to 48% at age 20 years, termed the survival cliff.
Outcomes in B-cell ALL has uncovered a biologic continuum across the age span.
Unfortunately, ALL subtypes commonly associated with a favorable prognosis, such as hyperdiploidy and ETV6-RUNX1, decrease in prevalence beyond childhood.
In contrast, many high-risk aberrations increase in prevalence with age beyond young adulthood, such as the Ph-positive BCR-ABL1 fusion and the KMT2A (MLL) rearrangements.
Several alterations are more common in the AYA age group.
Amplification of the long arm of chromosome 21 occurs in approximately 12% of AYAs between age 17 and 45 years and is associated with a poor prognosis.
Immunoglobulin heavy chain locus (IGH) rearrangements are relatively frequent in AYAs, peaking in incidence to 11% in the 20- to 24-year age group.
A high-risk subtype is Ph-like ALL, a biologically diverse entity that shares similar gene expression profiles to Ph-positive ALL but lacks the BCR-ABL1 fusion.
The prevalence of Ph-like ALL peaks in the AYA population, accounting for approximately 28% of AYA ALL as compared with approximately 10% of pediatric ALL and 20% of older adult ALL.
Ph-like ALL is typically associated with more aggressive disease, lower rates of minimal residual disease (MRD)–negative responses, and inferior survival.
Several newly described gene fusions are also more prevalent among AYAs: double homeobox 4 (DUX4) gene, zinc finger protein 384 (ZNF384), and myocyte enhancer factor 2D (MEF2D) rearrangements.
Front-Line AYA ALL Regimen studies demonstrated superior outcomes when AYAs were treated according to a pediatric protocol.
With a 3-year event-free survival (EFS) and overall survival (OS) of 59% and 73% (95% CI, respectively.
Median EFS was 78.1 months as compared with a historical control of 30 months.
Available data increasingly support the use of pediatric-inspired regimens to treat AYAs.
Pediatric protocols use higher cumulative doses of asparaginase, vincristine, and steroids; incorporate delayed intensification into the treatment schema; and provide more intensive CNS prophylaxis.
Pediatric-based regimens offer a lower cumulative dose of alkylators, anthracyclines, and cytarabine, which result in fewer long-term adverse effects, particularly infertility.
Asparaginase therapy in pediatric regimens carries a higher risk of hepatic, pancreatic, and thrombotic complications, and the risk is increased in older or obese patients.
Pediatric regimens are typically more complex than many adult regimens.
MRD has now become a standard of care in ALL across the age spectrum.
Measurement of MRD after completion of induction therapy aids in identifying AYAs without residual disease who on average will have excellent outcomes after pediatric therapeutic regimens.
The clinical utility of MRD measurement is not limited to only prognostication; MRD has now become an intervenable clinical end point.
Binatumomab, the bispecific monoclonal T-cell engager antibody that binds both CD3 and CD19, is
approved for the treatment of MRD-positive disease, and a number of clinical trials either accept MRD in the absence of morphological disease as an inclusion criterion or use MRD as a trial end point.
Methodologies exist for monitoring MRD, including flow cytometry, allele-specific oligonucleotide polymerase chain reaction, and next-generation sequencing of immunoglobulin and T-cell receptors.
Antibody-based and cellular therapies have become a new standard in the treatment of relapsed and/or refractory (R/R) B-cell ALL, greatly bolstering the armamentarium of therapeutic options.
Current immunotherapies specifically target cell surface antigens CD19, CD20, and CD22, which are expressed at a high level in pre-B ALL blast cells.
The antibody-based agents blinatumomab can serve as effective bridges to hematopoietic cell transplantation (HCT), whereas the role of chimeric antigen receptor (CAR) T-cell therapy in relation to HCT remains less well defined.
Blinatumomab has demonstrated remarkable efficacy in clinical trials.
Blinatumomab is approved by the FDA for MRD-positive disease, and is also approved for use in the R/R setting.
The international phase III TOWER study in patients with R/R Ph-negative ALL comparing blinatumomab versus standard salvage chemotherapy:
reported superior remission rates (45% v 25%, respectively;and median OS of 7.7 versus 4.0 months, respectively.
The most notable toxicities of blinatumomab are cytokine release syndrome and neurologic changes.
The risk of cytokine release syndrome is higher with greater tumor burden, but this can be mitigated through several approaches, including administering a lower dose of blinatumomab during the first week, pretreatment with steroids, lowering the disease burden before treatment, and holding additional doses or administering tocilizumab when symptoms arise.
FDA approval of Inovate for R/R B-cell ALL was based on the pivotal phase III INOVATE trial comparing IO versus standard salvage chemotherapy in patients with R/R ALL.
This study demonstrated a significantly higher remission rate (80.7% v 29.4%, longer progression-free survival of 5.0 versus 1.8 months and longer OS of 7.7 versus 6.7 months.with IO.
Veno-occlusive disease was a unique adverse event that occurred in 11% of IO-treated patients, as compared with 1% of patients treated with standard therapy.
Tisagenlecleucel is a CAR T-cell targeting CD19 approved by the FDA for the treatment of R/R B-cell ALL in patients up to age 25 years.
Approval of this agent phase II ELIANA trial of pediatric and young adult patients with CD19+ R/R B-cell ALL, which reported on survival outcomes of patients receiving CAR-T cell infusion.
In overall remission rate for patients receiving the CAR-T infusion was 81%, 95% of those in remission were MRD negative by 28 days post–CAR-T.
Six-month EFS and OS were 73% and 90%, respectively.
Cytokine release syndrome and neurotoxicity were common adverse events, occurring in 77% and 40% of patients, respectively; grade 3 or 4 cytokine release syndrome occurred in 45%, grade 3 neurotoxicity occurred in 13%, and there were no cases of grade 4 neurotoxicity:
risk of severe cytokine release syndrome and neurotoxic effects was increased with a higher disease burden.
The antibody agents blinatumomab and IO may be limited by shorter duration of response and survival outcomes, and currently HCT remains necessary for curative-intent treatment in the relapsed setting.
Data suggest a role for consolidative HCT after CAR T-cell therapy in patients with a short duration of B-cell aplasia (≤ 63 days), which is associated with increased risk of relapse.
Surface antigen loss or downregulation of either CD19 or CD22 is a major mechanism of resistance and relapse for both antibody-based and CAR T-cell therapy.
Bispecific CD19/CD22 CARs have been developed in response.
Results of a phase I study using CD19/CD22 CAR T cells in four pediatric patients with R/R ALL demonstrated safety and tolerability of the bispecific CAR as well as 100% remission rate with 75% MRD negativity.
HCT remains an important modality in curing Ph-negative ALL and is currently offered to patients in their second complete remission and beyond.
HCT is most commonly considered in AYAs in first remission with low-level MRD (typically after 10 to 16 weeks of intensive multi-agent chemotherapy) as well as those with high-risk biologic features, such as early T-cell precursor ALL or certain subsets of Ph-like ALL.
AYAs without high-risk features who are in MRD-negative remission should receive consolidative pediatric-inspired chemotherapy.
Reports of durable remissions after CAR T cells have called into question whether cure may be obtained after ALL relapse without allogeneic HCT.
Fertility preservation should be discussed with every AYA patient, because cancer treatments can cause temporary or permanent gonadal failure.
