Breathing, or ventilation, is the process of moving air out and in the lungs to facilitate gas exchange with the internal environment.
Breathing mostly flushes out carbon dioxide and brings in oxygen.
Oxygen is needed for cellular respiration, which uses the oxygen to break down foods for energy and produces carbon dioxide as a waste product.
Breathing, brings air into the lungs where gas exchange takes place in the alveoli through diffusion.
There is normally at rest a small alveolar-to-arterial O2 gradient of 1 to 5 mm Hg.
This mild gas exchange impairment is most likely the result of ventilation-perfusion mismatch or a small amount of shunted blood.
The circulatory system transports these gases to and from the cells, where cellular respiration takes place.
Breathing with lungs consists of repetitive cycles of inhalation and exhalation through a highly branched system of tubes or airways which lead from the nose to the alveoli.
The number of respiratory cycles per minute is the breathing or respiratory rate.
The respiratory rate and is one of the four primary vital signs of life.
Each breath temporal pattern at rest: inspiration takes a second or more and is accomplished almost exclusively by contraction of the diaphragm, whereas expiration at rest is passive and occurs due to the elastic recoil properties of the lung and chest wall.
During periods of increased ventilation, this pattern changes: inspiratory time shortens, additional inspiratory respiratory muscles are recruited to generate larger tidal volumes during exercise, and expiration can become active and aided by the muscles of the chest and abdomen.
One’s breathing depth and rate is automatically, and unconsciously, controlled by several homeostatic mechanisms.
These homeostatic mechanisms keep the partial pressures of carbon dioxide and oxygen in the arterial blood constant, contributing significantly to tight control of the pH of the extracellular fluids (ECF).
Over-breathing, hyperventilation, and under-breathing, hypoventilation, which decrease and increase the arterial partial pressure of carbon dioxide respectively.
Hyperventilation causes a rise in the pH of ECF.
Hypoventilation lowers the pH.
Breathing provides a mechanism for speech, laughter and expressions of emotions.
Breathing used for reflexes such as yawning, coughing and sneezing.
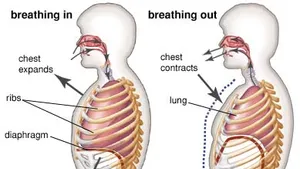
Contraction of the diaphragm generally contributes the most to the expansion of the chest cavity.
Intercostal muscles pull the ribs upwards also causing the rib cage to expand during inhalation.
The relaxation of all these muscles during exhalation causes the rib cage and abdomen to elastically return to their resting positions.
At rest, the tidal volume of each breath is roughly 500 mL.
About 150 to 200 mL of this breath represents dead space with 300 to 350 mL of alveolar ventilation available for gas exchange.
For most adults, activities that involve moderate exertion, with ventilation rates for adults that range from 35-45 liters/minute, include climbing stairs, playing tennis or baseball, simple garden or construction work, and brisk walking or light jogging, cycling, or hiking.
Activities that involve heavy exertion, with ventilation rates greater than 45 liters/minute for adults, include playing basketball or soccer, chopping wood, heavy manual labor such as digging in the garden, and vigorous running, cycling, or hiking.
In addition to a more forceful and extensive contraction of the diaphragm, the intercostal muscles are aided by the accessory muscles of inhalation to exaggerate the movement of the ribs upwards, causing a greater expansion of the rib cage.
During exhalation, in addition to relaxation of the muscles of inhalation, the abdominal muscles actively contract to pull the lower edges of the rib cage downwards decreasing the volume of the rib cage, while at the same time pushing the diaphragm upwards deep into the thorax.
The lungs are not capable of inflating themselves: they expand only when there is an increase in the volume of the thoracic cavity.
Lung inflation is achieved primarily through the contraction of the diaphragm, but also by the contraction of the intercostal muscles which pull the rib cage upwards and outwards.
During forceful inhalation the accessory muscles of inhalation, which connect the ribs and sternum to the cervical vertebrae and base of the skull, in many cases through an intermediary attachment to the clavicles, bring about a greater change in the volume of the chest cavity.
During exhalation, at rest, all the muscles of inhalation relax, returning the chest and abdomen to their resting position, which is determined by their anatomical elasticity.
During this exhalation point the lungs contain the functional residual capacity of air, which, in the adult human, has a volume of about 2.5–3.0 liters.
During heavy breathing, as in exercise, exhalation is brought about by relaxation of all the muscles of inhalation, but, in addition, the abdominal muscles, instead of being passive, now contract strongly causing the rib cage to be pulled downwards to the front and sides.
Vigorous exhalation decreases the size of the rib cage but also pushes the abdominal organs upwards against the diaphragm which consequently bulges deeply into the thorax.
The end-exhalatory lung volume will haven less air than the resting functional residual capacity.
In an adult human, there is always still at least one liter of residual air left in the lungs after maximum exhalation.
Diaphragmatic breathing causes the abdomen to rhythmically bulge out and fall back, and is referred to as “abdominal breathing”.
When the accessory muscles of inhalation are activated, as in during labored breathing, the clavicles are pulled upwards: sometimes referred to as clavicular breathing,
Clavicular breathing occurs especially during asthma attacks and in people with chronic obstructive pulmonary disease.
Ordinarily inhaled air is warmed and moistened by the wet, warm nasal mucosa: the air subsequently cools and dries.
When warm, wet air from the lungs is breathed out through the nose, the cold hygroscopic mucus in the cool and dry nose re-captures some of the warmth and moisture from that exhaled air.
In very cold weather the re-captured water may cause a dripping nose.
The nasal cavities are quite narrow, and divided in two by the nasal septum.
Nasal cavities’ lateral walls have several longitudinal folds, or shelves, called nasal conchae, exposing a large area of nasal mucous membrane to the air as it is inhaled and exhaled.
The nasal mucous membrane exposure to inhaled air, causes it to take up moisture from the wet mucus, and warmth from the underlying blood vessels, so that the air is nearly saturated with water vapor and is at almost body temperature by the time it reaches the larynx.
Conversely, part of this moisture and heat is recaptured as the exhaled air moves out over the partially dried-out, cooled mucus in the nasal passages, during exhalation.
The sticky mucus of the nasal mucosa traps much of the particulate matter that is breathed in, preventing it from reaching the lungs.
The upper airways include the nasal cavities, the pharynx, and larynx.
The lower airway is often described as a respiratory tree or tracheobronchial tree,
with larger airways give rise to branches that are slightly narrower, but more numerous than the airway that gives rise to the branches.
The human respiratory tree may consist of, on average, 23 such branchings into progressively smaller airways.
Proximal divisions of the lungs, trachea and bronchi, function mainly to transmit air to the lower airways.
Later divisions such as the respiratory bronchioles, alveolar ducts and alveoli are specialized for gas exchange.
The trachea and the first portions of the main bronchi are outside the lungs.
The tree branches within the lungs, and ultimately extends to every part of the lungs.
The alveoli are the blind-ended terminals of the respiratory tree.
Air that enters the alveoli has to exit the same way it came.
The respiratory system creates dead space: the volume of air that fills the airways at the end of inhalation, and is breathed out, unchanged, during the next exhalation, never having reached the alveoli.
The dead space is filled with alveolar air at the end of exhalation, which is the first air to breathed back into the alveoli during inhalation, before any fresh air which follows after it.
The dead space volume of a typical adult human is about 150 ml.
Breathing’s primary purpose of breathing is to refresh air in the alveoli so that gas exchange can take place in the blood.
The equilibration of the partial pressures of the gases in the alveolar blood and the alveolar air occurs by diffusion.
After exhaling, adult human lungs still contain 2.5–3 L of air:functional residual capacity (FRC).
With inhalation,about 350 mL of new, warm, moistened atmospheric air is brought in and is well mixed with the FRC.
The composition of the FRC changes very little during the breathing cycle.
With each breath the pulmonary, capillary blood always equilibrates with a relatively constant air composition in the lungs and the diffusion rate with arterial blood gases remains equally constant with each breath.
As a result tissues are not exposed to large swings in oxygen and carbon dioxide tensions in the blood caused by the breathing cycle: the peripheral and central chemoreceptors measure only gradual changes in dissolved gases.
The homeostatic control of the breathing rate depends on the partial pressures of oxygen and carbon dioxide in the arterial blood, which also maintains a constant pH of the blood.
The rate and depth of breathing is automatically controlled by the respiratory centers.
These respiratory centers receive information from the peripheral and central chemoreceptors, which
continuously monitor the partial pressures of carbon dioxide and oxygen in the arterial blood.
Central chemoreceptors are present on the surface of the medulla oblongata of the brain stem.
These chemoreceptors are sensitive to pH as well as the partial pressure of carbon dioxide in the blood and cerebrospinal fluid.
The second group of sensors measure the partial pressure of oxygen in the arterial blood, known as the peripheral chemoreceptors, and are situated in the aortic and carotid bodies.
Data from chemoreceptors is conveyed to the respiratory centers in the pons and medulla oblongata, which responds to fluctuations in the partial pressures of carbon dioxide and oxygen in the arterial blood by adjusting the rate and depth of breathing.
Chemoreceptor data transmitted to the respiratory centers above to restore the partial pressure of carbon dioxide to 40 mm Hg. the pH to 7.4 and, to a lesser extent, the partial pressure of oxygen to 100 mm Hg.
Exercise increases the production of carbon dioxide by the active muscles,
which diffuses into the venous blood and ultimately raises the partial pressure of carbon dioxide in the arterial blood.
The increased partial pressure of carbon dioxide in the arterial blood is immediately sensed by the carbon dioxide chemoreceptors on the brain stem.
The respiratory centers then respond by causing the rate and depth of breathing to increase to such an extent that the partial pressures of carbon dioxide and oxygen in the arterial blood return almost immediately to the same levels as at rest.
The respiratory centers communicate with the muscles of breathing via motor nerves.
The phrenic nerves, which innervate the diaphragm, are probably the most important of these muscles of breathing.
Automatic breathing can be overridden to a limited extent by choice to facilitate activities.
Conscious breathing practices promote relaxation and stress relief.
There are automatic breathing control reflexes:Submersion, particularly of the face, in cold water, triggers a response called the diving reflex.
The diving reflex shuts down the airways against the influx of water, the metabolic rate slows, there is intense vasoconstriction of the arteries to the limbs and abdominal viscera, reserving the oxygen that is in blood and lungs at the beginning of the dive almost exclusively for the heart and the brain.
The diving reflex is more effective in very young infants and children than in adults.
Exhaled air is breathed out through the mouth on a cold and humid conditions, the water vapor will condense into a visible cloud or mist.
Inhaled air is by volume 78% nitrogen, 20.95% oxygen and small amounts of other gases including argon, carbon dioxide, neon, helium, and hydrogen.
The gas exhaled is 4% to 5% by volume of carbon dioxide, about a 100 fold increase over the inhaled amount.
The volume of oxygen is reduced by a small amount, 4% to 5%, compared to the oxygen inhaled.
The typical composition of air:
5.0–6.3% water vapor
79% nitrogen
13.6–16.0% oxygen
4.0–5.3% carbon dioxide
1% argon
Atmospheric pressure decreases above sea level altitude, and the pressure in the alveoli/ lungs also decreases at the same rate with altitude.
Atmospheric pressure decreases exponentially with altitude, roughly halving with every 5,500 metres (18,000 ft) rise in altitude.
The composition of atmospheric air is, almost constant below 80 km, as a result of the continuous mixing effect of the weather.
The concentration of oxygen in the air decreases at the same rate as the atmospheric pressure.
At sea level, where the ambient pressure is about 100 kPa, oxygen contributes 21% of the atmosphere and the partial pressure of oxygen (PO2) is 21 kPa.
Even at the summit of Mount Everest, 8,848 metres (29,029 ft), where the total atmospheric pressure is 33.7 kPa, oxygen still contributes 21% of the atmosphere but its partial pressure is only 7.1 kPa
Therefore, a greater volume of air must be inhaled at altitude than at sea level in order to breathe in the same amount of oxygen in a given period.
During inhalation, air is warmed and saturated with water vapor as it passes through the nose and pharynx before it enters the alveoli.
The saturated vapor pressure of water is dependent only on temperature; at a body core temperature of 37 °C it is 6.3 kPa (47.0 mmHg), regardless of any other influences, including altitude.
The pressure gradient forcing air into the lungs during inhalation is reduced by altitude.
The lower viscosity of air at altitude allows air to flow more easily and this also helps compensate for any loss of pressure gradient.
At low atmospheric pressure on breathing normal accommodation occurs by auto,automatically increasing the volume of air breathed in — or out — per minute.
At low atmospheric pressure homeostatic mechanism prioritize the regulation of the arterial PCO2 over that of oxygen at sea level.
At sea level the arterial PCO2 is maintained at very close to 40 mmHg under a wide range of circumstances, at the expense of the arterial PO2, which is allowed to vary within a very wide range of values, before eliciting a corrective ventilatory response.
When atmospheric pressure falls to below 75% of its value at sea level, oxygen homeostasis is given priority over carbon dioxide homeostasis.
This switch-over occurs at an elevation of about 8,200 ft.
If this switch from pCO2 to O2/ occurs relatively abruptly, hyperventilation at high altitude will cause a severe fall in the arterial PCO2 with a consequent rise in the pH of the arterial plasma leading to respiratory alkalosis.
This is one factor contributing to high altitude sickness.
If the switch to oxygen homeostasis is incomplete, then hypoxia may complicate the clinical picture with potentially fatal results.
Pressure increases with the depth of water at the rate of about one atmosphere for every 10 meters.
Air breathed underwater by divers is at the ambient pressure of the surrounding water.
Breathing compressed gasses underwater may lead to several diving disorders which include pulmonary barotrauma, decompression sickness, nitrogen narcosis, and oxygen toxicity.
Air is provided by a diving regulator, which reduces the high pressure in a diving cylinder to the ambient pressure, to ease inhaling, so that breathing is effortless.
Many regulators have an adjustment to change the ease of inhaling so that breathing is effortless.
Abnormal breathing patterns include: Kussmaul breathing, Biot’s respiration and Cheyne–Stokes respiration.
Breathing disorders include: dyspnea, stridor, apnea, sleep apnea, mouth breathing, and snoring.
Hypopnea refers to overly shallow breathing.
Hyperpnea refers to fast and deep breathing brought on by a demand for more oxygen, as for example by exercise.
The terms hypoventilation and hyperventilation also refer to shallow breathing and fast and deep breathing respectively
During physical exercise, a deeper breathing pattern is adapted to facilitate greater oxygen absorption.
During deep breathing, the thoracic diaphragm adopts a lower position in the core and this helps to generate intra-abdominal pressure which strengthens the lumbar spine.
Typically, this allows for more powerful physical movements to be performed. As such, it is frequently recommended when lifting heavy weights to take a deep breath or adopt a deeper breathing pattern.

 See Lungs
See Lungs