
 JIA encompasses a heterogeneous group of disorders.
JIA encompasses a heterogeneous group of disorders.
Classification describes seven types of illness: oligoarticular arthritis, polyarticular arthritis (rheumatoid factor positive and rheumatoid factor negative types) , enthesitis related arthritis, psoriatic arthritis, undifferentiated with rightists, and systemic arthritis.
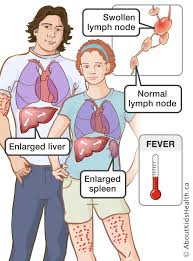
Characterized by chronic arthritis, systemic manifestations of fevers, rash, hepatosplenomegaly, lymphadenopathy, serositis, and increased inflammatory markers.
Juvenile idiopathic arthritis is the most common childhood rheumatic disease.
JIA prevalence between 16-150 per 100,000.
In the severest subtype patients experience unremitting chronic polyarthritis.
Systemic arthritis is one of the least common and most severe type.
Systemic arthritis accounts for 5- 15% of newly diagnosed juvenile idiopathic arthritis.
Systemic arthritis often develops in children younger than five years of age although it occurs at all ages.
Patients with systemic arthritis are often ill.
Systemic arthritis is associated with fever, characteristically on a daily basis with 1 to 2 spikes in temperature.
Systemic arthritis is associated with the evanesceny macular rash whenthe temperature is high.
Its arthritis is usually polyarticular and can involve large in small joints.
Arthritis may not appear for weeks or even months after the onset of the disease.
Laboratory abnormalities associated with systemic juvenile idiopathic arthritis include: leukocytosis, neutrophilia, anemia, thrombocytosis, elevated ESR and C reactive protein, D dimer, and ferritin levels.
Autoantibodies such as rheumatoid factor, cyclic citrullinated peptide, anti-neutrophil cytoplasmic antibody, and anti-nuclear antibody are generally not found.
Patients sustain joint damage and disabilities.
Complications of the process include growth in impairment, the development of osteoporosis, and potentially the lethal macrophage activation syndrome.
Increased levels of interleukin-6 in serum and synovium correlated with clinical and lab abnormalities.
Interleukin-6 excessive production is a factor in the pathogenesis of the disease.
Interleukin-1 has also been implicated in the pathogenesis of the disease.
Patients may be susceptible to infections because of immunosuppressive effects of the disease or its management.
Treatment for systemic arthritis is aimed at controlling the systemic features and the arthritis.
Glucocorticoids can lead to significant improvement but are associated with toxic effects.
Interleukin1- inhibitors, and interleukin6-inhibitor tocilizumab have proven very effective.
40% of patients have a monophasic course of disease with remission, and a small percentage have recurrent periods of active disease/quiescence.
Over half the patients have ongoing arthritis even if systemic features subside.
Patients with prolonged disease may require methotrexate, abatacept, and tumor necrosis factor Inhibitors.
10% of patients with systemic juvenile idiopathic arthritis can develop macrophage activation syndrome manifested by fever, hepatic dysfunction, purpura, CNS involvement and multi organ system failure.
Among children with JIA who had undergone primary immunizations, the MMR booster vaccination was not associated with adverse outcomes of the disease activity (Heijstek MW et al).
2
